Primary cutaneous anaplastic large-cell lymphoma
Published Web Location
https://doi.org/10.5070/D34n62v82wMain Content
Primary cutaneous anaplastic large-cell lymphoma
Tracey Newlove MD, Aaron Loyd MD, Rishi Patel MD, Josef Jelinek MD, Jo-Ann Latkowski MD
Dermatology Online Journal 16 (11): 2
Department of Dermatology, New York University, New York, New YorkAbstract
Primary cutaneous anaplastic large-cell lymphoma (ALCL) is a form of cutaneous T-cell lymphoma that is characterized by solitary or localized nodules or plaques. Histopathologic features include a diffuse, non-epidermotropic infiltrate with cohesive sheets of large anaplastic CD30+ tumor cells. This entity must be distinguished from systemic ALCL with cutaneous involvement and lymphomatoid papulosis. Treatment modalities include clinical monitoring, radiation therapy, and surgical excision, with systemic chemotherapy reserved for disseminated or extracutaneous disease.
History
 |
| Figure 1 |
|---|
A 90-year-old man presented to the Dermatologic Associates at NYU Langone Medical Center in April, 2005, for evaluation of an asymptomatic, shiny, brown papule on the inner aspect of the left thigh. A biopsy specimen obtained at that time disclosed the diagnosis and a wide local excision was performed. The patient was followed without recurrence until December, 2008, when he developed several, indurated plaques and nodules on the lateral aspect of the left shin. Biopsy specimens confirmed recurrence. These lesions were clinically monitored until September, 2009, when he developed an enlarging nodule with ulceration. Treatment with intralesional triamcinolone acetonide, 10 mg/ml, was administered without improvement. Subsequently, localized radiation therapy was initiated.
Past medical history included anemia of chronic disease, chronic renal insufficiency, hypertension, cardiac arrhythmia, hepatitis C virus infection, glaucoma, cataracts, and arthritis. Current medications include dutasteride, allopurinol, aspirin, amitryptyline, hydrochlorothiazide, labetalol, bimatoprost, amlodipine, and erythropoietin alfa. He does not currently use tobacco, alcohol, or illicit substances.
Physical examination
Multiple, pink-brown, shiny, indurated plaques and nodules were present on the lateral aspect of the left shin and anterior tibial surface. The largest lesion was ulcerated centrally. There were no similar lesions elsewhere on body. There was no cervical, axillary, or inguinal lymphadenopathy or hepatosplenomegaly.
Laboratory data
Flow cytometry analysis of peripheral blood performed in April, 2005, showed no immunophenotypic evidence of lymphoma or leukemia, with normal expression of B- and T-cell antigens and a normal CD4/CD8 ratio. PET-CT scan of the chest, abdomen, and pelvis in April, 2005, was negative.
Histopathology
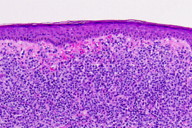 |
| Figure 2 |
|---|
Within the dermis there are diffuse sheets of enlarged cells with pleomorphic nuclei and ample amphophilic cytoplasm. The epidermis is uninvolved. There is focal papillary dermal edema (Figure 2). A CD30 immunostain shows diffuse reactivity of greater than 75 percent of lymphocytes (Figure 2, inset).
Comment
Primary cutaneous anaplastic large-cell lymphoma (ALCL) is a form of cutaneous T-cell lymphoma (CTCL) and is recognized by the WHO-EORTC classification as an indolent cutaneous CD30+ lymphoproliferative disorder [1]. Anaplastic large-cell lymphomas were first recognized as a distinct entity in 1985 and consist of cells with an anaplastic, pleomorphic, or immunoblastic cytomorphology and expression of the CD30 antigen by the majority (more than 75%) of tumor cells [2]. Within this group there are currently three distinct clinical entities: primary systemic anaplastic lymphoma kinase (ALK)-positive ALCL, primary systemic ALK-negative ALCL, and primary cutaneous ALCL [3].
Primary cutaneous ALCL affects older patients, with a median age of 60 years and a male-to-female ratio of between 2 and 3 to 1. It accounts for approximately 9 percent of cutaneous lymphomas. Approximately 25 percent of patients show partial or complete spontaneous regression [4]. Primary cutaneous ALCL has a favorable prognosis, with a five-year disease specific survival of 95 percent, compared with 79.8 percent for ALK+ systemic ALCL and 32.9 percent for ALK− systemic ALCL [1].
The disease usually presents as a solitary, asymptomatic nodule or plaque, with or without superficial ulceration. Less common presentations include multiple, localized nodules or multicentric tumors at disseminated sites. Extracutaneous dissemination is observed in approximately 10 percent of cases and usually manifests as regional lymphadenopathy.
Histopathological findings include a diffuse, non-epidermotropic infiltrate with cohesive sheets of large CD30+ tumor cells. Classically the tumor cells have the characteristic morphology of anaplastic cells and show round, oval, or irregularly-shaped nuclei; prominent eosinophilic nucleoli; and abundant cytoplasm; however, a pleomorphic or immunoblastic appearance is observed in 20 to 25 percent of cases [5].
The main differential diagnoses include lymphomatoid papulosis, systemic anaplastic large-cell lymphoma with cutaneous involvement, or large-cell transformation of mycosis fungoides. It is now generally accepted that lymphomatoid papulosis (LyP) and primary cutaneous ALCL are entities on the same spectrum of CD30+ proliferative disorders. To distinguish ALCL from LyP, longitudinal observation often is necessary. LyP presents as small, erythematous papules with necrosis, which appear in crops that wax and wane over time. ALCL presents with larger nodules that do not appear in crops.
Initial management of suspected ALCL includes aPET-CT scan and flow cytometry analysis to distinguish limited cutaneous disease from systemic disease with cutaneous involvement. Immunohistochemistry study for ALK also should be performed as ALK expression is almost invariably absent from cutaneous CD30+ lymphoproliferative disorders [6].
Currently accepted treatment modalities for primary cutaneous ALCL include observation, surgical excision, or local radiation. In cases with a large tumor burden, rapid progression of skin lesions, or extracutaneous involvement, systemic chemotherapy with low-dose methotrexate or doxorubicin may be considered.
References
1. Willemze R, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768. [PubMed]2. Stein H, et al. The expression of the Hodgkin disease associated antigen Ki-1 in reactive and neoplastic lymphoid tissue: evidence that Reed-Sternberg cells and histiocytic malignancies are derived from activated lymphoid cells. Blood 1985;66:848. [PubMed]
3. Stein H, et al. CD30+ anaplastic large cell lymphoma: a review of its histopathologic, genetic, and clinical features. Blood 2000;96: 3681 [PubMed]
4. Bekkenk MW, et al. Primary and secondary cutaneous CD30+ lymphoproliferative disorders; a report from the Dutch Cutaneous Lymphoma Group on the long term follow-up data of 219 patients and guidelines for diagnosis and treatment. Blood 2000; 95: 3653 [PubMed]
5. Willemze R, et al. EORTC classification for primary cutaneous lymphomas: a proposal from the Cutaneous Lymphoma Study Group of the European Organization for Research and Treatment of Cancer. Blood 1997;90:354 [PubMed]
6. Pulford K, et al. Nucleophosmin (NPM)-ALK proteins in normal and neoplastic cells with detection of anaplastic lymphoma kinase (ALK) and nucleolar protein the monoclonal antibody ALK1. Blood 1997;89:1394 [PubMed]
© 2010 Dermatology Online Journal

