Dyshidrosiform Pemphigus vulgaris: Report of an unusual case
Published Web Location
https://doi.org/10.5070/D34j17s91dMain Content
Dyshidrosiform Pemphigus vulgaris: Report of an unusual case
Ramesh C Gharami MD1, Piyush Kumar MD2, Avijit Mondal MD2, Kalyan Ghosh MD2
Dermatology Online Journal 16 (7): 10
1. Associate professor, Dermatology, Medical College, Kolkata, India. 2. PG student, Dermatology, Medical College, Kolkata. India. docpiyush@gmail.com
Abstract
Dyshidrosiform Bullous pemphigoid is a well-known entity, but dyshidrosiform pemphigus vulgaris has rarely been described. Our patient, a 36-year-old female, with a known case of pemphigus vulgaris (PV) for the last 6 years, presented with a 3 month history of a dyshidrosiform eruption of the soles. On the basis of histopathological and direct immunofluorence (DIF) findings, the new eruption was diagnosed as PV. We report our case as dyshidrosiform pemphigus vulgaris.
Introduction
Pemphigus vulgaris (PV) is characterized clinically by flaccid vesicles/bullae and erosions of skin and mucosa and histologically by suprabasal clefting and acantholytic cells on histopathology [1]. However, the presentation may be altered when the patient has been on irregular and/or low doses of corticosteroids that are inadequate to control the disease. Our case, a known PV patient, was self-medicating with irregular and low doses of prednisolone (30-40 mg per day). She presented with a dyshidrosiform eruption of the soles and oral erosions, plus a few vesicles elsewhere. Such a presentation has rarely been described with PV.
Case
A 36-year-old female patient presented with a 3-month history of vesicles and bullae with extensive crusting over both soles. She also exhibited a few bullae on the body and erosions of the oral mucosa.
She was a known case of PV for the last six years and had been admitted twice in the hospital for this. In her last hospital admission, she was treated with dexamethasone in the hospital and oral prednisolone after discharge; she was lost to follow-up. When she returned with the new eruptions, she revealed that she had been self-medicating with prednisolone, approximately 30 to 40 mg per day, when she developed lesions and ceasing when she became lesion free.
She came to us with the above presentation after a period of 1½ years from the last hospital admission. At this time she reported that she had been taking 30 mg per day for 2 weeks. On examination, the oral mucosa and extremities were involved more severely than the trunk. Her soles were heavily crusted with vesicles and bullae, both discrete and confluent, especially at the margin. The dorsal feet were relatively spared. Palm involvement was significantly less as compared to soles and was in the form of a few discrete vesicles and pustules only. The trunk had a few vesicles and bullae over normal appearing skin. Both the bulla spreading sign and the Nikolsky sign were positive. The oral mucosa had extensive erosions and hemorrhagic crusts. The rest of the mucocutaneous examination was unremarkable. Routine investigations did not reveal any abnormality. Gram stain as well as KOH mount from a lesion did not reveal any organism.
 |  |
| Figure 3 | Figure 4 |
|---|---|
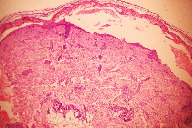
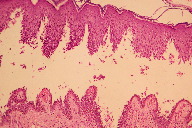
| Figure 3. Histopathology photograph showing intraepidermal blister (H&E, x40) Figure 4. Histopathology photograph showing “classical row of tombstones” appearance (H&E, x100) | |
The condition was diagnosed as pemphigus vulgaris with dyshidrosiform involvement of the soles based on histopathology and DIF findings. Histopathology showed intra epidermal blistering with classical “row of tombstones” appearance with prominent acantholytic cells and few neutrophils and eosinophils.
 |
| Figure 5 |
|---|
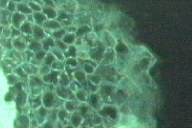
| Figure 5. DIF photograph showing Deposition of Ig G (and hence fluorescence) along the cell margin throughout the epidermis |
Direct immunofluorence from the perilesional skin was diagnostic. It showed deposition of IgG on the cell surface of entire epidermis.
She was treated with prednisolone 80 mg per day and cyclophosphamide 50 mg per day along with symptomatic therapy. She improved within 2 weeks and was discharged.
The dose of prednisolone is being tapered slowly, continuing cyclophosphamide at the same dose. The patient is still under follow up (6 months from presentation) and no recurrence has been noted so far.
Discussion
Dyshidrosiform eczema (Pompholyx) is a well-known condition and is characterized by extremely pruritic deep-seated vesicles on the sides (i.e., lateral and medial aspects) of the fingers, palms, and soles [2]. It can be idiopathic or associated with various disorders. On the other hand, similar involvement of palms and soles can be seen in various conditions including vesicobullous disorders like BP. It is interesting to note that both BP and PV have been included in the differential diagnosis of vesicobullous eruption of palm and sole [3]. While dyshidrosiform BP is a widely accepted entity [4], dyshidrosiform PV is rarely mentioned.
Palm and/or sole involvement in pemphigus vulgaris is quite rare. Masala et al. have reported palm involvement in a 58-year-old PV patient and have observed that palm involvement was associated with aggressive behavior of the PV [5]. A similar prognostic importance of palm involvement is also reported by Vaishnani et al. [6]. Borradori et al. have reported PV presenting as pompholyx of the left foot [7]. Bolling et al. [8] have reported a unique case with palmoplantar keratoderma and a pemphigus-like immunobullous disorder, with antibody against Desmocollin 3 (not against Desmoglein 3). However, none of them reports a classical dyshidrosiform involvement. To the best of our knowledge, there is only one prior case report of dyshidrosiform pemphigus [9].
Our case had a prominent vesicobullous eruption of palms and soles with few lesions elsewhere. Apart from a prior diagnosis of PV and irregular self-medication with prednisolone, her history was unremarkable. There was no aggravating factor. We have seen many relapse episodes of PV presenting initially as PF or BP when patients are on inadequate corticosteroid therapy (irregular and/or low). It seems corticosteroids at inadequate (low) dosages are ineffective in containing the relapse. But they do alter the clinical presentation. The unique presentation in our case may be explained by inadequate and irregular medication. Histopathology and DIF proves the diagnosis of PV. With this case report we intend to increase the awareness of such a presentation to avoid delay in diagnosis and proper management. It should be considered when the patient has a vesicobullous eruption of palms and soles along with vesicles and bullae elsewhere, especially the oral mucosa. Also we suggest that dyshidrosiform PV should be considered as a defined variant of PV.
References
1. Stanley JR. Pemphigus. In : Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell D J, editors. Fitzpatrick's Dermatology in General Medicine. 7th ed. New York: McGraw-Hill publications; 2008. 459-672. Miller JL, Hurley HJ. Diseases of the Eccrine and Apocrine Sweat Glands. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2nd ed. Spain : Mosby Elsvier limited; 2008.
3. Doshi DN, Kimball AB. Vescicular palmoplantar eczema. In : Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell D J, editors. Fitzpatrick's Dermatology in General Medicine. 7th ed. New York: McGraw-Hill publications; 2008. 162-6
4. Stanley JR. Bullous pemphigoid. In : Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell D J, editors. Fitzpatrick's Dermatology in General Medicine. 7th ed. New York: McGraw-Hill publications; 2008. 475-80
5. Masala MV, Cozzani E, Rosella M, Montesu MA. Pemphigus vulgaris on palms. European J Dermatol 1997; 6: 453-4.
6. Vaishnani JB, Bosamiya SS. Pemphigus: Active or inactive? Indian J Dermatol 2009;54:186-8 [PubMed]
7. Borradori L, Harms M. Podopompholyx due to pemphigus vulgaris and Trichophyton rubrum infection. Report of an unusual case. Mycoses 2009; 37: 137-9. [PubMed]
8. Bolling MC, Mekkes JR, Goldschmidt WF, Van Noesel CJ, Jonkman MF, Pas HH. Acquired palmoplantar keratoderma and immunobullous disease associated with antibodies to desmocollin 3. Br J Dermatol. 2007 Jul; 157(1):168-73.
9. Milgraun SS. Pemphigus vulgaris masquerading as dyshidrotic eczema. Cutis 1985; 35: 445-6.
© 2010 Dermatology Online Journal





