Diffuse plane xanthomata
Published Web Location
https://doi.org/10.5070/D34d80p34qMain Content
Diffuse plane xanthomata
Jennifer Bragg MD
Dermatology Online Journal 11 (4): 4
Department of Dermatology, New York University School of Medicine
Abstract
An 80-year-old woman presented with yellow-orange papules and plaques on her scalp, back, and arms, with a Koebner reaction of the lesions on her back. Clinical and histopathologic findings were consistent with the diagnosis of diffuse plane xanthoma. Laboratory data showed normal lipid levels and an abnormal paraprotein in the blood. A bone marrow biopsy specimen was normal. Diffuse plane xanthoma is frequently associated with reticuloendothelial disorders, which may appear several years after the skin findings. Treatment is limited but may include the use of ablative lasers.
An 80-year-old woman presented to the Charles C. Harris Skin and Cancer Pavilion for a second opinion regarding treatment options for her condition. She reported yellow-orange lesions that first appeared on her upper back and then spread to her scalp and arms over the next few months. She complained of mild pruritus and was concerned that the lesions might continue to spread. Past medical history includes hypertension and irritable-bowel syndrome. She denied a family history of similar skin lesions or cancers. Treatment with triamcinolone ointment 0.1 percent had no effect. A biopsy confirmed the diagnosis.
Yellow-orange, flat-topped papules and plaques were noted on the scalp, proximal arms, and upper back, with a single lesion behind each ear. On the lateral upper back, the lesions were distributed in a vertical linear array underneath the patient's bra straps. The axillae and face, including the eyelids, were spared.

|
|
| Figure 1 | Figure 2 |
|---|
A complete blood count, comprehensive metabolic panel, fasting lipid panel, and urinalysis were normal. An IgG monoclonal protein was identified on serum protein electrophoresis. A bone marrow biopsy specimen and aspirate showed a normocellular marrow with 7-10 percent plasma cells but no definite light chain restriction.
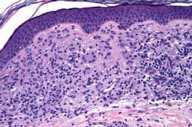
Histopathology revealed within the papillary dermis there is a nodular proliferation of foamy histiocytes admixed with lymphocytes and scattered Touton giant cells. The overlying epidermis is normal.
Comment
Diffuse normolipemic plane xanthoma (DPX) was described in 1962 [1]. Three major features were identified: xanthelasma; diffuse plane xanthoma of the head, neck, trunk, and extremities; and normal plasma lipid levels. Xanthelasma typically appear first (although not in this case), followed by involvement of the lateral parts of the neck and upper trunk. The lesions are symmetrically distributed, asymptomatic, yellow-to-brown patches or plaques, which may involve flexural areas as well as scars. In this case, the isomorphic response was apparent. This association has been reported in one case of eruptive xanthomas [2], but never in DPX. On histopathologic examination, foam cells (macrophages that have engulfed lipid droplets) and variable numbers of Touton giant cells, lymphocytes, and foamy histiocytes can be seen [3].
Some 4 years after the first description of DPX, an association with reticuloendothelial disorders, especially multiple myeloma and monoclonal gammopathy, was reported [4]. Since then, a case series [3] found reticuloendothelial disease in three of eight patients, which suggested a lower than expected incidence of underlying disease. Interestingly, the three patients with an underlying disorder had more extensive skin involvement than did the others. Despite the findings in this case series, periodic monitoring for myeloproliferative disorders is still recommended, as these associated conditions may develop several years after the appearance of the xanthomas [5].
The pathogenesis of DPX has not been clearly defined. Several theories have been suggested. Some authors believe that paraprotein-lipoprotein complexes are deposited in the skin. Others suggest that leukemic cells infiltrate the skin with subsequent xanthomatization. Still others consider that DPX is a form of non-X histiocytosis.
In patients with limited involvement, the individual lesions can be excised. Other options include chemabrasion, dermabrasion, and ablative laser therapy. The erbium:YAG laser has been used successfully to treat facial xanthomas in one patient [6].
References
1. Altman J, et al. Diffuse normolipemic plane xanthoma. Arch Dermatol 1962;85:6332. Scavo S, et al. Isomorphic response in eruptive xanthomas. Dermatology 2004;209:66
3. Marcoval J, et al. Diffuse plane xanthoma: clinicopathologic study of 8 cases. J Am Acad Dermatol 1998;39:439
4. Lynch PJ, et al. Generalized plane xanthoma and systemic disease. Arch Dermatol 1966;93:639
5. Loo DS, et al. Diffuse normolipidemic plane xanthomas with monoclonal gammopathy presenting as urticarial plaques. J Am Acad Dermatol 1996;35:829
6. Lorenz S, et al. Treatment of diffuse plane xanthoma of the face with the Erbium:YAG laser. Arch Dermatol 2001;137:1413
© 2005 Dermatology Online Journal

