Paraneoplastic Acanthosis Nigricans: The importance of exhaustive and repeated malignancy screening
Published Web Location
https://doi.org/10.5070/D34603s4fmMain Content
Paraneoplastic Acanthosis Nigricans: The importance of exhaustive and repeated malignancy screening
Narmita Talsania MBBS MRCP, Catherine A Harwood MBBS MA PhD MRCP, D Piras, Rino Cerio FRCP (Lond) FRCP (Edin) FRCPPath
Dermatology Online Journal 16 (8): 8
Barts and The London NHS Trust, London UK, and Queens Hospital, Romford, Essex, UKAbstract
Paraneoplastic acanthosis nigricans (P-AN) characteristically has a sudden onset, rapid progression, and extensive cutaneous involvement. The association between P-AN and internal malignancy is well established and the most common association is with adenocarcinoma of gastrointestinal origin. We present the case of an 81-year-old man with a 12-month history of anorexia, weight loss, and clinical evidence of extensive acanthosis nigricans. After exhaustive and repeated investigations a papillary thyroid carcinoma and a follicular adenoma were identified and he improved upon its resection. To our knowledge, P-AN in association with thyroid neoplasm has been reported on only one previous occasion.
Introduction
We report a case of malignant acanthosis nigricans presenting with extensive mucocutaneous involvement; the underlying neoplasm was a follicular thyroid carcinoma, a malignancy rarely reported in association with paraneoplastic acanthosis nigricans.
Case report
An 81-year-old man presented with a 12-month history of anorexia, weight loss of 12 kg, and generalized thickening and hyperpigmentation of his skin. His past medical history included myocardial infarction and atrial fibrillation for which he had been taking ramipril, sotalol, and warfarin.
 |  |
| Figure 1a | Figure 1b |
|---|---|
| Figures 1a and 1b. Verrucous hyperkeratosis and thickening of skin of both axillae | |
 |  |
| Figure 2a | Figure 2b |
|---|---|
| Figures 2a and 2b. Tylosis of both palms | |
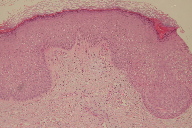
Examination revealed generalized erythroderma with pronounced nipple hyperkeratosis, periocular skin thickening, verrucous hyperkeratosis of both axillae (Figures 1a and 1b), thickening of palmar skin (Figures 2a and 2b), leukokeratosis of the tongue (Figure 3), and longitudinal nail ridging. A skin biopsy from the lateral neck showed irregular acanthosis, hyperkeratosis, and hypergranulosis with minimal inflammation (Figure 4).
On the basis of these clinical and pathological findings, a diagnosis of generalized acanthosis nigricans caused by suspected underlying malignancy was made. Of note, he had nuclear radiation exposure in Hiroshima in 1945.
An extensive screen for occult malignancy was performed, but initially proved negative. Circulating tumor markers were normal. Whole body CT scan showed no evidence of underlying malignancy. Gastritis and duodenitis were observed on upper gastrointestinal endoscopy, but barium swallow and chest x-ray did not identify any abnormalities.
Despite treatment with topical steroids and salicylic acid, his condition failed to improve and the search for malignancy continued. Within 9 months, repeat tumor markers had become abnormal; CA19-9 was now elevated to 61 ku/L (normal<35); CEA had increased to 4.6 microg/L (normal<3.4). ESR was also now 97mm/hr (normal=1-10). Repeat CT scan suggested enlarged hilar lymph nodes. A mediastinoscopic hilar lymph node biopsy was normal, excluding Hodgkins disease and lung cancer. The lymph node did not show any feature of Castleman disease. Bronchoscopy and repeat upper gastrointestinal endoscopy with gastric biopsy were also normal. However, T4 was low 8.0 pmol/L (normal=10.5-24.5). TSH and thyroglobulin were within normal range and PET/CT showed increased uptake in the left thyroid region. Fine needle aspiration from a thyroid nodule confirmed a follicular thyroid neoplasm.
He underwent surgery for his thyroid neoplasm. Histology confirmed papillary carcinoma in the left lobe of the thyroid and follicular adenoma in the right lobe. Six months following the operation the patient’s skin had significantly improved and he was stable.
Discussion
Paraneoplastic acanthosis nigricans (P-AN) characteristically has a sudden onset, rapid progression, and extensive cutaneous involvement, as seen in our patient [2]. Occasionally it may be present on the mucous membranes of the oral cavity, nasal and laryngeal mucosa, and esophagus, with papillomatous lesions on the eyelids and conjunctiva.
Paraneoplastic acanthosis nigricans has been reported with many kinds of cancer, but by far the most common underlying malignancy is adenocarcinoma of gastrointestinal origin, usually gastric adenocarcinoma [2]. To our knowledge, P-AN in association with follicular thyroid neoplasm has been reported on only one previous occasion with a follicular adenocarcinoma of the thyroid gland arising in a patient with congenital hypothyroidism [1]. CA 19-9, the tumor-associated antigen most significantly elevated in our patient, is raised in pancreatic, upper gastrointestinal, hepatobiliary obstruction, and thyroid disease. CEA is raised in normal adults, pregnant women, smokers, and in thyroid cancer patients [6].
Regression of P-AN has been observed when the underlying malignancy is treated. Conversely, its reappearance may suggest recurrence or metastasis of the primary tumor [3]. The prognosis for patients with P-AN is often poor and the average survival time is 8.7 to 11.9 months [4].
The molecular mechanisms responsible for the clinicopathologic manifestations of P-AN are not fully understood. It has been proposed that epidermal growth factor (EGF) secreted by the tumor binds to EGF receptors and this, in turn, activates the AKt pathway known to be involved in keratinocyte proliferation and epidermal thickening. Interestingly, AKt pathway overactivation is common in thyroid cancer (particularly follicular thyroid cancer) [5].
This case highlights the importance of exhaustive and repeated investigations in the search for underlying malignancy in patients with extensive mucocutaneous acanthosis nigricans.
References
1. Verdich J. Acanthosis nigricans Associated with Adenocarcinoma of the Thyroid gland. Dermatologica. 1980; 161:355-360. [PubMed]2. Weger W, Ginter-Hanselmayer G, Hammer HF, et al. Florid cutaneous papillomatosis with acanthosis nigricans in a patient with carcinomas of lung and prostate. J Am Acad Dermatol. 2007; 57(5):907-908. [PubMed]
3. Longhsore S, Taylor J, Kennedy A, et al. Malignant acanthosis nigricans and endometrioid adenocarcinoma of the parametrium: the search for malignancy. J Am Acad Dermatol. 2003; 49(3):541-543. [PubMed]
4. Kebria M, Belinson J, Kim R, et al. Malignant acanthosis nigricans, tripe palms and the sign of Leser-Tre'lat, a hint to the diagnosis of early stage ovarian cancer: A case report and review of the literature. Gynaecologic Oncology. 2006; 101(2):353-355. [PubMed]
5. Ringel MD, Hayre N, Saito J, et al Overexpression and Overactivation of Akt in Thyroid Carcinoma. Cancer Res. 2001; 61:6105-11. [PubMed]
6. Gorgone S, Lazzara S, Palmeri R, et al. Use of tumour markers in monitoring thyroid carcinoma. Chirurgia Italiana. 1987; 39(1):87-95. [PubMed]
© 2010 Dermatology Online Journal