Syringocystoadenoma papilliferum associated with apocrine hidrocystoma and verruca
Published Web Location
https://doi.org/10.5070/D341n0k2vgMain Content
Syringocystoadenoma papilliferum associated with apocrine hidrocystoma and verruca
Salvador Arias-Santiago MD1, Pedro Aceituno-Madera MD1, Jose Aneiros-Fernández MD2, María Teresa Gutiérrez-Salmerón PhD1, Ramón Naranjo-Sintes PhD1
Dermatology Online Journal 15 (11): 9
1. Department of Dermatology. San Cecilio University Hospital. Granada, Spain. salvadorarias@hotmail.es2. Department of Pathology. San Cecilio University Hospital. Granada, Spain
Abstract
Syringocystoadenoma papilliferum is a benign adnexal tumor usually located in head and neck that occurs during childhood or adolescence. A case of a syringocystoadema papilliferum associated with apocrine hydrocystoma and verruca is presented. It is unusual to see the occurrence of three histopathologic types of tumors coexisting in one cutaneous lesion.
Introduction
Syringocystoadenoma papilliferum is a benign adnexal tumor, usually located in head and neck, that occurs during childhood or adolescence. It usually presents as a papule or a group of papules distributed linearly. Nodular or verrucous transformation is noted at puberty. The uncommon sites of presentation are upper arms, chest, scrotum, thigh, male breast, and eyelids [1, 2]. Histological examination reveals ducts connecting with the epidermis, containing papillary processes, and lined by two epithelial cell layers. A case of a syringocystoadema papilliferum associated with apocrine hydrocystoma and verruca is presented.
Case report
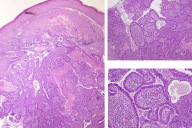
A healthy 19-year-old man with no contributory past medical history, was referred to our clinical with a three-year history of asymptomatic papules and nodules on the chest that had grown recently. There was no bleeding, but there were serous secretions on some surfaces. A physical examination showed multiple firm, non-tender papules and nodules located on the pre-sternal area; they were linearly arranged with a yellowish secretion on the surface. The tumors had a palpable deep component with an elastic consistency. At the bottom there were also other papular lesions with a keratotic surface and a linear arrangement (Fig. 1). No other similar lesions were observed on the patient's face, trunk, or extremities and no systemic disease was reported. The patient's family did not have any similar cutaneous lesions. Laboratory tests including blood count, biochemistry, coagulation tests, and CRP were normal. Chest radiographs were unremarkable and the ultrasound scan showed a 2.5 x 2.5 cm soft tissue mass in the subcutaneous tissue under the nodular lesion.
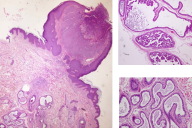
Syringocystoadenoma papilliferum associated with subcutaneous angioma and molluscum lesions were suspected after clinical examination. Several biopsies were performed and histopathologic examination was compatible with syringocystoadenoma papilliferum (ducts connecting to the surface, containing papillary processes and line by two epithelial cell layers) associated with verruca and subjacent apocrine hidrocystoma (Figs. 2 & 3). We determined the presence of HPV-6 in the lesions. After histological confirmation, surgical excision of all the lesions were performed.
Discussion
It is unusual to see the occurrence of three histopathologic types of tumor coexisting in one cutaneous lesion. Syringocystadenoma papilliferum and apocrine hidrocystoma are benign sweat gland tumors that usually occur separately. The origin of syringocystoadenoma papilliferum is controversial, an apocrine derivation has been postulated because the cells lining the lumina show decapitation secretion. Despite this, the tumor is rare in the axilla and immunohistochemistry studies are not conclusive. Others authors have suggested that the tumor represents an adenoma of ecrine duct origin or that it is derived from eccrine or apocrine glands. One third of all cases arise in an organoid nevus sebaceus of Jadassohn [3]; coexisting basal cell carcinoma is noted in 10 percent of the cases. Less frequently it has been associated with other histopathologic types of sweat gland tumor such as tubular apocrine adenoma, papillary eccrine adenoma, mixed tubulopapillary hidradenoma [4], sebaceous carcinoma, trichoadenoma, trichoblastoma, trichilemmoma, hidradenoma papilliferum and apocrine hidrocystoma.
We highlight in this case the association of three different types of tumor and the atypical location of the syringocystoadenoma papilliferum. Two theories have been proposed to explain the association with hidrocystoma, the first one is that all cells of these two histopathologic types arose from multipotential undifferentiated cells, which then differentiated toward two lines of differentiation. The second theory is that syringocystadenoma papilliferum was the only existing histopathologic type initially and then activation of primitive cells in the syringocystadenoma papilliferum resulted in the formation of the apocrine hidrocystoma. Also syringocystoadenoma papilliferum can be associated with HPV infections such as condyloma acuminatum [5, 6]; in the present case it was associated with a verruca, HPV-6 positive.
Surgical excision of this tumor is recommended because malignant transformation has been described. Clinical clues to malignant changes are rapid growth, ulceration, pruritus and pain [7]. CO2 laser excision or Mohs surgery are other therapeutic options [8].
References
1. Malhotra P, Singh A, Ramesh V. Syringocystadenoma papilliferum on the thigh: an unusual location. Indian J Dermatol Venereol Leprol. 2009;75:170-2. [PubMed]2. Vaos G, Pierrakou P. Syringocystadenoma papilliferum: a rare breast tumor in a young boy. Pediatr Dev Pathol. 2006;9:381-3. [PubMed]
3. Premalata CS, Kumar RV, Malathi M, Shenoy AM, Nanjundappa N. Cutaneous leiomyosarcoma, trichoblastoma, and syringocystadenoma papilliferum arising from nevus sebaceus. Int J Dermatol. 2007;46:306-8. [PubMed]
4. Hsu PJ, Liu CH, Huang CJ. Mixed tubulopapillary hidradenoma and syringocystadenoma papilliferum occurring as a verrucous tumor. J Cutan Pathol. 2003;30:206-10. [PubMed]
5. Skelton HG 3rd, Smith KJ, Young D, Lupton GP. Condyloma acuminatum associated with syringocystadenoma papilliferum. Am J Dermatopathol. 1994;16:628-30. [PubMed]
6. Coyne JD, Fitzgibbon JF. Mixed syringocystadenoma papilliferum and papillary eccrine adenoma occurring in a scrotal condyloma. J Cutan Pathol. 2000 ;27:199-201. [PubMed]
7. Park SH, Shin YM, Shin DH, Choi JS, Kim KH. Syringocystadenocarcinoma papilliferum: a case report. J Korean Med Sci. 2007;22:762-5. [PubMed
8. Chi CC, Tsai RY, Wang SH. Syringocystadenocarcinoma papilliferum: successfully treated with Mohs micrographic surgery. Dermatol Surg. 2004 ;30:468-71. [PubMed]
© 2009 Dermatology Online Journal