Case Report: Diffuse plane xanthoma with low C4 and systemic inflammatory symptoms
Published Web Location
https://doi.org/10.5070/D33p17h4jxMain Content
Case Report: Diffuse plane xanthoma with low C4 and systemic inflammatory symptoms
Alejandro Malbrán1, Luz Stella Parra2, José G Casas3, Eloisa Malbrán4, Elena Yeyati4, Gabriel Magariños3, Mario A Marini2
Dermatology Online Journal 15 (4): 5
1. Immunology Department, Hospital Británico de Buenos Aires2. Dermatology Department, Hospital Británico de Buenos Aires
3. Pathology Service, Hospital Británico de Buenos Aires
4. Unidad de Alergia, Asma e Inmunología Clínica, Buenos Aires, Argentina. eloisamalbran@gmail.com
Abstract
A normolipemic patient with diffuse plane xanthomas, IgG monoclonal gammopathy of unknown significance, low levels of C4, and systemic inflammatory symptoms is presented. Delay from disease onset to diagnosis is discussed.
Introduction
Diffuse normolipemic plane xanthomatosis (DNPX) was first described by Altmann and Winkelmann in 1962 [1]. It is a rare form of xanthomatosis, clinically characterized by yellowish-orange plaques that may affect any part of the body. Since its original description, it has been recognized to be associated with hematological diseases, especially with multiple myeloma and monoclonal gammopathy [2].
We describe a patient with diffuse plane xanthoma, low C4, inflammatory symptoms, and monoclonal gammopathy. There was significant delay to final diagnosis even in the presence of extensive cutaneous involvement.
Case report
A 64-year-old man had a 7-year history of episodes of arthritis and fever, lasting up to 48 hours that affected his shoulders, elbows, ankles, and wrist joints. He was diagnosed with palindromic rheumatism and was treated successfully with corticosteroids and hydroxycloroquine. At the time of onset of his rheumatological symptoms, he also first noted an extensive, but subtle, yellow and orange discoloration of the skin. The skin changes were not recognized as being significant by his physicians at that time. Two years later he developed recurrent episodes of panniculitis (lobular), affecting lower and upper limbs, abdomen and thorax; he was treated with high doses of methotrexate, systemic corticosteroids, and non-steroidal inflammatory drugs. He had a normal complete blood count and routine chemistry, but he had remarkably elevated acute phase reactants and undetectable C4. Three years prior to presentation to the dermatology clinic, an IgG monoclonal gammopathy of unknown significance was discovered. During the past year an episode of autoimmune sudden deafness was diagnosed.
 |  |
| Figure 1 | Figure 2 |
|---|
The patient was referred to the dermatology clinic seven years after the onset of his joint and skin condition. On physical exam, yellow-orange discoloration was noted on the right hemithorax and waist (Figs. 1 & 2). The patient did not exhibit xanthelasma. A skin biopsy of a discolored area was performed.
 |
| Figure 3 |
|---|
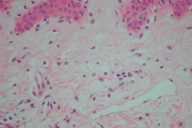
The skin biopsy showed proliferation of vacuolated histiocytes within the papillary dermis with a normal overlying epidermis, confirming the clinical diagnosis of diffuse plane xanthomas (Fig. 3).
Relevant laboratory tests were performed including C1Q, C1INH, C4 and C3 levels, which were measured by radial immunodifusion. The results are presented in Table 1.
The diagnosis of DNPX was made.
Conclusions
Since its first description, the diagnosis of DNPX was based on three major features: 1) diffuse plane xanthomas of the head, neck, trunk, and extremities, 2) palpebral xanthelasma, 3) normal plasma lipid levels [3]. It affects both sexes, between 40 and 60 years of age. Hofmann et al. [4] reported a pediatric case, which was diagnosed at three months of life. The infant exhibited yellow-brown plaques, mainly on his trunk. Skin lesions are described as yellowish-orange macules or slightly elevated plaques of different sizes, with diffuse or sharply demarcated borders [2, 5, 6]. The first signs generally begin in the face with palpebral xanthelasmas. Later skin involvement slowly progresses to involve other areas of the body. Lesions on mucous membranes are infrequent.
Four years after its description in 1962, Lynch and Winkelmann [3] detected a strong association of DNPX with systemic disorders, especially with multiple myeloma and monoclonal gammapathy (Table 2) [7, 8]. It is suggested that extensive cutaneous involvement may be indicative of the presence of an underlying systemic disease [9].
The pathogenesis of this entity remains uncertain. In the cases of DNPX associated with monoclonal gammopathy, as seen in our patient, the lipid deposits in the skin are postulated to be due to the formation of immune complexes of the monoclonal IgG and low density lipoproteins (LDL). These immune complexes are deposited in the skin and later phagocytosed by histiocytes. The first investigations that mention the anti-lipoprotein activity of the paraproteins were reported in 1965, in the extensive studies of Beaumont et al. [10, 11]. Taylor et al. [12], in 1978, suggested the association of paraproteins with DNPX. Since then, 21 cases with multiple myeloma and xanthomatosis have been confirmed as having lipoprotein-paraprotein complexes. The rate of lipid deposition appears to be determined by the properties of the complex rather than the serum lipid levels. This explains why the majority of the cases of DNPX are normolipemic [4, 5, 6].
Other immunological abnormalities found in patients with DNPX are complement alterations, such as increased activation and consumption. The case reported here had undetectable C4 and diminished C1 IHN and C1Q. The consumption of C4 would be explained by two mechanisms: 1) the presence of paraproteins that activate the complement via the classical pathway, leading to the consumption of C4 and 2) an acquired deficiency of C1 IHN. Jordon et al. [13]. and Yu et al. [14] reported several cases with DNPX associated with acquired deficiency of C1 INH. Besides this acquired deficiency, these patients had low levels of C1, C4, and C2. C1 is constantly produced in the blood; low levels of C1 INH lead to a constant activity of C1 upon its substrate C4, leading to low serum levels of C4.
The lesions of DNPX may also exhibit purpura or petechiae. This may be a result of vasculitis due to the deposition of immune complexes or paraprotein aggregates [5].
Diffuse normolipemic plane xanthomatosis must be differentiated from Montgomery Syndrome or xanthoma disseminatum. This syndrome was first described by Montgomery and Osterberg [15]. It represents a rare disorder with few cases reported in the literature. This condition mainly affects young male adults, who are normolipemic, and show the following triad: 1) papular or patchy xanthomatous lesions localized on flexures or eyelids, 2) diabetes insipidus in 40 percent of the cases due to hypothalamic/hypophyseal compromise, and 3) xanthomas on mucous membranes and in the upper respiratory tract [16, 17].
Therapeutic strategies for DNPX patients are scarce. In patients with limited involvement, like palpebral xanthelasmas, treatments that include excision or ablative laser therapy may be offered [18]. The extensive lesions in our patient precluded any local treatment.
References
1. Altman J, Winkelmann RK. Diffuse normolipemic plane xanthoma: generalized xanthelasma. Arch Dermatol 1962;85:633-640. [PubMed]2. Massengale WT, Nesbitt Jr LT. Xanthomas En Bolognia JL, Jorizzo JL, Rapini RP. Dermatología. Copyright 2004, Elsevier España, SA. P.4451-52.
3. Lynch PJ and Winkelmann RK. Generalized plane xanthomas and systemic disease. Arch Dermatol 1966; 93:639-646. [PubMed]
4. Hofmann M, Zappel K, Trefzer U, et al. Diffuse normolipemic plane xanthoma in a 9- year old boy. Ped Dermatol 2005;22(2):127-29. [PubMed]
5. Russel Jones R, Baughan ASJ, CreamJJ, et al. Complement abnormalities indiffuse plane xanthomatosis with paraproteinaemia. Br J Dermatol 1979; 101:711-15. [PubMed]
6. Modiano P, Gillet-Terver MN, Relchert S, et al. Normolipemic plane xanthoma, monoclonal gammapathy, antilipoprotein activity, hypocomplementemia, Ann Dermatol Venereol 1995; 122: 507-08. [PubMed]
7. Gómez Centeno P, Garcia Acosta A, Rodriguez Lopez JA y col. Xantoma plano difuso asociado a gammapatía monoclonal, crioglobulinemia e hipocomplementemia. Actas Dermosifiliogr 2001; 92: 97-100.
8. Trasobares Marugan L, Vera Castaño A, Del Valle Martin M y col. Xantomas planos difusos normolipémicos asociados a gammapatía monoclonal IgG L. Revisión de la literatura. Actas Dermosifiliogr 1989; 11:818-824.
9. Marcoval J, Moreno A, Bordas X y col. Diffuse plane xanthoma: clinicopathologic study of 8 cases. J Am Acad Dermatol 1998, 39: 439-42. [PubMed]
10. Beaumont JL, Jacotot B, Beaumont V, et al. Myelome, hyperlipidemie et xanthomatose. Nouv Rev Franc Hemat 1965; 5: 507-517. [PubMed]
11. Beaumont JL, Beaumont V, Antonnucci M, et al. Les auto-anticorps antilipoprotéines de miélome: Etude coparée deux typex: L'IgA anti-Lp P.G. et l'IgG anti-Lp A.S. Ann Biol Clin 1970; 28:387-399. [PubMed]
12. Taylor JS, Lewis LA, Battle Jr J D et al. Plane xanthoma and multiple myeloma with lipoprotein-paraprotein complexing. Arch Dermatol 1978; 114: 425-31. [PubMed]
13. Jordon RE, McDuffer FC, Good RA, Day NK. Diffuse normolipaemic plane xanthomatosis: an abnormal complement component profile. Clin Exp Immunol 1974;18: 407-15. [PubMed]
14. Yu HS, Ishibashi Y, Kukita A. A case of diffuse plane xanthomatosis. J of Dermatol 1980; 7:247-254. [PubMed]
15. Montgomery H, Osterberg AE. A correalation of clinical, histopathologic and clinical studies of cutaneous xanthomas. Arch Dermato Syph 1938; 37: 473-502.
16. Altman J, Winkelmann RK. Xanthoma disseminatum. Arch Dermatol 1962; 86:582-86.
17. Mishkel MA, Cockshott WP, Nazir DJ, et al. Xanthoma disseminatum. Clinical, metabolic, pathological and radiological aspects. Arch Dermatol 1977; 113: 1094-100. [PubMed]
18. Lorenz S, Hohenleutner S, Hohenleutner U et al. Tretament of diffuse plane xanthomas of the face with the Erbium :Yag Laser. Arch Dermatol 2001; 137: 1413-15. [PubMed]
© 2009 Dermatology Online Journal

