Adult-onset linear syringocystadenoma papilliferum over the inguinal fold: A case report with emphasis on mast cell staining pattern
Published Web Location
https://doi.org/10.5070/D33dk440q1Main Content
Adult-onset linear syringocystadenoma papilliferum over the inguinal fold: A case report with emphasis on mast cell staining
pattern
Sudip Kumar Ghosh MD DNB, Rajesh Kumar Mandal MD, Debabrata Bandyopadhyay MD, Sramana Mukhopadhyay Mukhopadhyay DDVL MD
Dermatology Online Journal 18 (11): 16
R G Kar Medical College, Kolkata, West Bengal, IndiaAbstract
Syringocystadenoma papilliferum (SCAP) is a rare hamartoma with predominant apocrine differentiation. Clinically, presenting as solitary nodule, nodular plaque, or linear nodules, SCAP usually occurs over the head and neck region in children. Out of these three morphological presentations, the linear type is the most rare. We report herein a case of a 36-year-old man with linear SCAP over the right inguinal fold, for its rarity. Besides the typical histologic features, a marked increase in lesional mast cell concentration as compared to a control specimen obtained from an unaffected site and a strikingly raised number of spreading and degranulated mast cells were demonstrated.
Introduction
Syringocystadenoma papilliferum (SCAP) is a benign hamartoma, an adnexal tumor with predominantly apocrine differentiation. They usually present at birth or early childhood and are usually located over the head and neck region. SCAP may occur de novo or over an organoid nevus like nevus sebaceus [1]. Morphologically, SCAP presents as a solitary nodule, nodular plaque, or linear nodules that may become verrucous and crusted at puberty. Although the clinical presentation of SCAP is varied, the histology is quite uniform and forms the basis of the diagnosis. It has been observed that there may be a marked increase of the mast cell count in the stroma of benign cutaneous tumors [2]. However, such data pertaining to SCAP is lacking.
Linear SCAP is an uncommon condition [3] and is even more rare outside the head and neck region. We report here a case of linear SCAP over the right inguinal region in a young man. Furthermore, we investigated the mast cell staining pattern of the tumor in our case.
Case report
A 36-year-old man presented with multiple dome-shaped, non-tender, and non-pruritic nodules on his right inguinal fold. The lesions appeared on normal-looking skin 15 years prior to presentation and had gradually increased in number and size over the last few years. Off late, the patient had noticed rapid enlargement and irregularity of the surface of some of the nodules with oozing of blood-tinged fluid, prompting him to seek medical advice. He had applied some topical preparations of unclear composition without any effect. There was no systemic symptom and no suggestive drug history.
Examination revealed multiple skin-colored, dome-shaped, firm, non-tender nodules over the right inguinal fold in a linear fashion (Figure 1). The size of the individual lesions varied from 1 cm x 1 cm to 2 cm x 2 cm. Whereas most of the lesions were smooth-surfaced, some had a warty surface with surface erosion. A serosanguinous discharge was evident at places (Figure 2). The rest of the skin was normal and there was no regional lymphadenopathy. The largest nodule was excised.
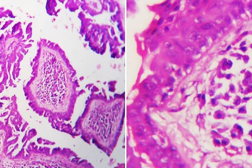
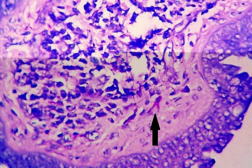
Histopathological examination (Figure 3) of the excised specimen showed hyperplastic epidermis and the presence of multiple cystic, papillary, and ductal invaginations extending into the dermis. These invaginations were connected to a hyperkeratotic and acanthotic epidermis. A double layer of cells consisting of an outer layer of cuboidal cells and an inner luminal layer of tall columnar cells were seen lining the invaginations. The connective tissue core was filled with plasma cells. Based on the clinical and histological findings, a diagnosis of linear SCAP was made. A toludine blue staining (Figure 4) showed a marked increase (in comparison to the mast cell concentration of a control specimen obtained from his normal skin) in the number of spreading and degranulated mast cells in the underlying papillary and reticular dermis and also in the stromal core of the papillae within the cystic invaginations (Table 1). The patient was sent for plastic surgery consultation and was offered surgical excision with skin grafting. The excised specimen also showed the histological picture of SCAP.
Discussion
Syringocystadenoma papiliferum (SCAP) is usually present at birth or early childhood [1]. Seventy five percent of the cases have been reported in the head and neck region, occurring de novo or associated with nevus sebaceus. However, a few cases of SCAP occurring outside the head and neck region have also been reported [3, 4, 5]. SCAP has very rarely been reported in the inguinal region [6, 7].
The other unusual sites of occurrence include chest, arms, breast, eyelids, axilla, scrotum, lower limb, perineal regions, and back [3-7]. Furthermore, only a few cases of linear SCAP have been reported [1]. Nearly all the cases of linear SCAP involved the neck, and less frequently, the chest, arm, and thigh. The linear variant of SCP is usually present at birth or at infancy [8]. Linear SCP on the inguinal region occurring in an adult was the interesting combination of features in our patient.
SCAP may be associated with apocrine poroma, apocrine acrosyringeal keratosis, apocrine hidrocystoma, tubular apocrine adenoma, papillary eccrine adenoma, eccrine nevus, tubulopapillary hidroadenoma, hidroadenoma papilliferum, linear nevus verrucosa, atypical fibroxanthoma, basal cell epithelioma, sebaceous epithelioma, trichoepithelioma, verruca vulgaris, and nevus comedonicus [7]. However, our patient did not have any such association.
Clinically, certain conditions can mimic linear SCAP. These include linear epidermal nevus, nevus comedonicus, basaloid follicular hamartoma, viral warts, eccrine nevus, verrucous carcinoma, subcutaneous fungal infection, and tuberculosis verrucosa cutis. Histopathologic features ruled out these possibilities in our patient.
Histopathological examination of SCAP [1] shows multiple cystic invaginations extending downwards from the epidermis. The upper portions of the invaginations are lined by squamous, keratinizing cells. In the lower portion of cystic invaginations, multiple papillary projections extend into the lumen of the invaginations. These papillary projections and the lower portion of the invaginations are lined by glandular epithelium typically consisting of two rows of cells. The inner luminal row consists of columnar cells and sometimes shows active decapitation secretion. In many cases there may be groups of tubular glands with large lumina in the deep dermis beneath the cystic invaginations [1]. One significant and diagnostic feature is the presence of a cellular infiltrate mainly composed of plasma cells within the stroma of this tumor, particularly in the papillary projections. There is increasing evidence in favor of an apocrine differentiation of this tumor. However an eccrine differentiation may occur in a few cases of SCAP [1].
Marked increase of the mast cell count in the stroma of benign cutaneous tumors was reported previously [2]. Increased mast cell degranulation was also noted in cutaneous appendageal tumors [9]. We could not, however, find any such data pertaining to SCAP in the PubMed database. Our patient showed a marked increase in the total mast cell concentration in the lesional skin as compared to a control specimen. Additionally, the spreading and degranulated mast cells were strikingly raised in the excised specimen of SCAP.
Large numbers of mast cells are present in several benign skin tumors such as neurofibromas. These mast cells may contribute directly to neurofibroma growth. Mast-cell blockers, such as ketotifen have been shown to retard this growth [10]. It would be interesting to see if similar benefit could be obtained in other cutaneous tumors including SCAP, which show increased mast cell density.
Malignant transformation to basal cell carcinoma, squamous cell carcinoma, or sweat gland carcinoma has been reported in plaque, solitary, and nodular variants of SCAP. However, malignant transformation usually does not occur in case of linear SCAP, probably because of their de novo origin [8].
Surgical excision is the treatment of choice for SCAP [11]. Carbon dioxide laser can be a useful treatment option for lesions on anatomic sites not suitable for surgery [8, 11]. We report the present case because of its combination of a few rare features, such as the unusual location, linear arrangement, and late-onset of the lesion. We also emphasize that linear SCAP should be considered in the differential diagnosis of any case which presents with linear nodules. Additionally, the pattern of mast cell staining was a hitherto unreported observation in SCAP.
References
1. Weedon D. Weedon’s Skin Pathology. 3rd ed. Philadelphia: Churchill Livingstone-Elsevier; 2010.2. Cawley EP, Hoch-Legeti C. Association of tissue mast cells and skin tumors. Arch Derm 1961; 83: 92-6. [PubMed]
3. Patterson JW, Straka BF, Wick MR. Linear syringocystadenoma papilliferum of the thigh. J Am Acad Dermatol 2001;45: 139-41. [PubMed]
4. Ghosh SK, Bandyopadhyay D, Chatterjee G, Bar C. Syringocystadenoma papilliferum: an unusual presentation. Pediatr Dermatol 2009; 26:758-9. [PubMed]
5. Rao VA, Kamath GG, Kumar A. An unusual case of syringocystadenoma papilliferum on the eyelid. Indian J Ophthalmol 1996; 44: 168-9. [PubMed]
6. Pahwa P, Kaushal S, Gupta S, Khaitan BK, Sharma VK, Sethuraman G. Linear syringocystadenoma papilliferum: an unusual location. Pediatr Dermatol 2011; 28:61-2. [PubMed]
7. Yap F B, Lee B R, Baba R. Syringocystadenoma papilliferum in an unusual location beyond the head and neck region: A case report and review of literature. Dermatol Online J 2010; 16(10): 4. [PubMed]
8. Martorell-Calatayud A, Sanz-Motilva V, Garcia-Sales MA, Calatayud-Blas A. Linear syringocystadenoma papilliferum: an uncommon event with a favorable prognosis. Dermatol Online J. 2011; 17(8):5. [PubMed]
9. Kim CS, Lee YB. Mast cell changes in skin diseases. Yonsei Med J 1978; 19:16-24. [PubMed]
10. Riccardi VM. Mast-cell stabilization to decrease neurofibroma growth. Preliminary experience with ketotifen. Arch Dermatol 1987; 123:1011-6. [PubMed]
11. Taylor RS, Perone JB, Kaddu S, Kerl H. Appendage Tumors and Hamartomas of the Skin. In: Wolf K, Goldsmith LA, Katz SI, Gilcrest BA, Paller AS, Leffel DJ. editors. Fitzpatrick’s Dermatology in General Medicine. New York: McGraw-Hill. pp 1068-87.
© 2012 Dermatology Online Journal