An Unusual Tumor of the Forearm
Published Web Location
https://doi.org/10.5070/D33dg4w9txMain Content
An Unusual Tumor of the Forearm
Rebecca Lu BA, Richard A. Krathen MD, Ramsey F. Markus MD
Dermatology Online Journal 12 (1): 13
Baylor College of Medicine, Houston, Texas. Rmarkus@bcm.tmc.eduClinical synopsis
 |
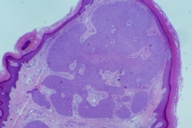
| Figure 1 |
|---|
| Figure 1. Pink papule on the ventral forearm. |
A 76-year-old man was referred to the VA Medical Center dermatology clinic for a 2-month history of a lesion on the right forearm. This growth was asymptomatic. However, the patient noted occasional minor bleeding. There had been no preceding therapy for this lesion prior to his visit to dermatology. The patient also noted a distant history of vitiligo that had remained stable. He was not currently receiving treatment for his vitiligo.
Physical examination revealed a healthy man appearing slightly younger than his stated age. There was a 7-mm fleshy pink pedunculated papule on the right ventral forearm (Fig. 1). There were no other relevant findings on examination.
A biopsy from the right ventral forearm was performed.
Microscopic findings
 | 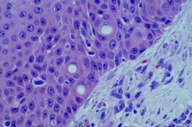 |
| Figure 2 | Figure 3 |
|---|---|
| Figure 2. Well-circumscribed nodules of basaloid cells in the dermis. | |
| Figure 3. Uniform basaloid cells with eosinophilic cytoplasm forming duct-like structures. | |
Skin biopsy specimen shows the epidermis with compact orthokeratosis and partial attenuation of the normal rete ridge pattern. In the dermis there are multiple well-circumscribed nodules composed of uniform basaloid cells with eosinophilic cytoplasm, some of which are forming duct-like structures. There is no cytologic atypia and no mitotic figures are seen (Figs. 2 and 3). The histologic findings were consistent with a dermal duct tumor.
Discussion
Dermal duct tumor clinically has a nonspecific appearance. It can be skin colored, pigmented, smooth, shiny, variegated, or scaly. Although it is often found on the head and neck [1, 2], its presence on the extremities [3, 4] and trunk [5, 6, 7] is not uncommon. Crusting or ulceration may occur secondary to clinical or subclinical trauma [1]. The differential diagnosis on presentation is broad and can include nevus, skin tag, cyst, basal cell carcinoma, verruca vulgaris, hemangioma, pyogenic granuloma, dermatofibroma, and a variety of adnexal tumors [1, 2].
Previously classified as a distinct entity [3, 5, 6], the dermal duct tumor is now believed to be a variant of the poroma [1, 4, 8, 9]. Poromas are benign neoplasms of sweat glands and are composed of cuboidal poroid cells, eosinophilic cuticular cells, and glycogen-rich clear cells [4, 8]. The etiology is unknown, but it has been suggested that the major neoplastic cell involved is the poroid cell, which can differentiate into cuticular and clear cells [4, 8]. Recent evidence shows that poromas can derive from both eccrine and apocrine sweat glands [10].
There are four variants of poromas as follows: eccrine poroma, hidroacanthoma simplex, dermal duct tumor, and poroid hidradenoma. In general, they are distinguished based on cytologic appearance of the cells and degree of epidermal and dermal involvement [4, 8, 9]. Eccrine poroma involves the epidermis and superficial dermis and is composed of a mixture of poroid, cuticular, and clear cells. Hidroacanthoma simplex is limited to the epidermis and consists of mostly poroid cells, a small amount of cuticular cells, and usually lacks clear cells. The dermal duct tumor is limited to the dermis and is composed of a mixture of all three types of cells. This variant can have small foci of solid or cystic components. Poroid hidradenoma is also confined to the dermis but, unlike the small foci seen in dermal duct tumors, it has large aggregates of solid and cystic components. Two or more of the above variants can exist in the same lesion [4].
Histopathology of the dermal duct tumor shows intradermal masses of poroid, clear, and cuticular cells formed around ductal structures [4]. Clear cells are distinguished from poroid cells by having a large amount of PAS-positive, diastase-resistant glycogen granules [4]. Poroid cells have only a small amount of these glycogen granules. Cystic spaces filled with an amorphous eosinophilic material may also be present. These cystic spaces are not lined with an epithelium and do not contain keratin [2, 4]. Histochemistry of the tumor demonstrates staining for phosphorylase, periodic acid-Schiff (PAS), adenosine triphosphatase, succinic dehydrogenase, cytochrome oxidase, and keratin [2, 4]. It is also partially positive for ferritin and CEA [4]. The tumor cells do not stain for β-glucuronidase, alkaline phosphatase, acid phosphatase, nonspecific esterase, indoxyl esterase, or leucine aminopeptidase [2, 4].
This dermal duct tumor was removed by shave biopsy followed by electrofulguration of the base. It has not recurred to date. Because of the nonspecific clinical presentation and broad body surface distribution of the dermal duct tumor, a biopsy is strongly recommended to confirm the diagnosis and rule out porocarcinoma, the malignant counterpart of the poroma. Definitive treatment is surgical excision; recurrence is rare [3].
References
1 Moore TO, Orman HL, Orman SK, Helm KF. Poromas of the head and neck. J Am Acad Dermatol 2001; 44:48-52. PubMed2 Hu CH, Marques AS, Winkelmann RK. Dermal duct tumor: a histochemical and electron microscopic study. Arch Dermatol. 1978;114:1659-64. PubMed
3 Apisarnthanarax P, Mullins JF. Dermal duct tumor. Arch Dermatol 1975; 111:1171-3. PubMed
4 Kakinuma H, Miyamoto R, Iwasawa U, Baba S, Suzuki H. Three subtypes of poroid neoplasia in a single lesion: eccrine poroma, hidroacanthoma simplex, and dermal duct tumor. Histologic, histochemical, and ultrastructural findings. Am J Dermatopathol 1994; 16:66-72. PubMed
5 Winkelmann RK, McLeod WA. The dermal duct tumor. Arch Dermatol 1966; 94:50-5. PubMed
6 Aloi FG, Pippione M. Dermal duct tumor. Appl Pathol 1986; 4:175-8. PubMed
7 Lintner R, Ilyas EN, Elder D, Heymann W. Nodule on the back of a 73-year-old woman--case. Arch Dermatol. 2004 May;140(5):609-14. PubMed
8 Abenoza P, Ackerman AB. Neoplasms with eccrine differentiation. Philadelphia: Lea & Febiger; 1990. p. 113-85.
9 Rutten A, Requena L, Requena C. Clear-cell porocarcinoma in situ: a cytologic variant of porocarcinoma in situ. Am J Dermatopathol 2002; 24:67-71. PubMed
10 Harvell JD, Kerschmann RL, LeBoit PE. Eccrine or apocrine poroma? Six poromas with divergent adnexal differentiation. Am J Dermatopathol 1996; 18:1-9. PubMed
© 2006 Dermatology Online Journal

