Cutaneous cholesterol embolization syndrome: A case report
Published Web Location
https://doi.org/10.5070/D33d11w0pbMain Content
Cutaneous cholesterol embolization syndrome: A case report
Nibedita Patro1 MD, Renu George1 MD, Pradyumn Singh2 MD, George Joseph3 MD DM
Dermatology Online Journal 18 (7): 10
1. Department of Dermatology, Christian Medical College, Vellore, Tamilnadu, India2. Department of Pathology, Christian Medical College, Vellore, Tamilnadu, India
3. Department of Cardiology, Christian Medical College, Vellore, Tamilnadu, India
Abstract
An 81-year-old woman with chronic kidney disease, systemic hypertension, and a large infra-renal abdominal aortic aneurysm, developed bilateral calf muscle pain, altered sensorium, and deterioration of renal function following endovascular aneurysmal repair. On the third post-operative day she developed symmetrical purpuric macules with erythematous margins on the gluteal region and bluish reticulated patches on the soles and tips of toes. This was followed by melena development on the seventh post-operative day. Histology of the skin confirmed the diagnosis of cutaneous cholesterol embolization syndrome (CES). She was treated with hemodialysis and supportive management and she recovered.
Introduction
Cholesterol embolization syndrome (CES) is caused by embolization of cholesterol crystals from atherosclerotic plaques lining the walls of major arteries. Cutaneous manifestations are the most common physical findings allowing early diagnosis [1].
Case report
 |  |
| Figure 1A | Figure 1B |
|---|
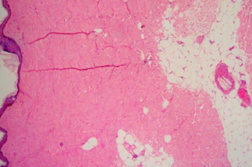
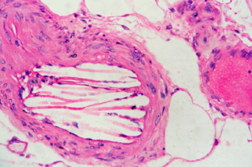
An 81-year-old woman with chronic kidney disease and hypertension underwent an endovascular repair for an abdominal aortic aneurysm. Twenty-four hours later she complained of bilateral calf muscle pain and developed altered sensorium with deterioration of renal function. On the third post-operative day she developed symmetrical purpuric macules with erythematous margins of sizes ranging from 4 x 5 cm to 10 x 7 cm on the gluteal region (Figure 1A) and bluish reticulated patches on the soles and tips of toes (Figure 1B). This was followed by melena. Abnormal laboratory parameters included a decrease in hemoglobin from 10.2 gm/dL (at admission) to 6.5 gm/dL, leukocytosis of 13,700/mm³, serum creatinine of 2 mg/dL (0.5-1.4 mg/dL) increasing to 3.1 mg/dL, serum urea, 85 mg/dL (15-40 mg/dL) increasing to 116 mg/dL, amylase, 212 U/L (28-100 U/L), creatine kinase, 1274 U/L (45-195 U/L), serum aspartate aminotransferase, 126 U/L (8-40 U/L), serum alanine aminotransferase, 43 U/L (5-35 U/L), and erythrocyte sedimentation rate, 87 mm/hour. Doppler sonography of both lower limbs for deep vein thrombosis and a CT scan of the brain were normal. A skin biopsy from the periphery of the lesion on the gluteal area showed an arteriole in the subcutis with typical needle-shaped (cholesterol) clefts (Figures 2A and 2B) and an unremarkable epidermis and dermis confirming the diagnosis of CES. The patient recovered with hemodialysis and supportive management.
 |  |
| Figure 2A | Figure 2B |
|---|
Discussion
The two main clinical manifestations of CES are peripheral cutaneous involvement and acute renal insufficiency [2]. The precise clinical syndrome depends on the location of the source of embolism. Since the abdominal aorta is the most common location of atherosclerosis, the kidneys, visceral organs, and lower extremities are commonly involved [2] as seen in our patient. Atheromas of other arteries, such as the ascending aorta or the carotid, may result in emboli, producing neurologic, retinal, or cardiac symptoms [1]. The risk factors for CES include advanced age, smoking, hypertension, diabetes mellitus, hyperlipidemia, and peripheral vascular disease. CES is seen following invasive vascular procedures as in our patient, thrombolytic therapy, or anticoagulants but may occur spontaneously as well.
In one study, cutaneous manifestations were reported in 88.5% of patients [1]. These included livedo reticularis (49%), gangrene (35%), cyanosis (28%), ulceration (17%), nodules (10%), and purpura (9%) [3]. Skin biopsy is diagnostic in 92% of the cases [2, 4] and it must include an area between middle to deep dermis. The needle-shaped spaces left by the dissolved crystals within the lumen of arterioles from affected skin are characteristic.
Laboratory investigations tend to be nonspecific, with raised ESR, microcytic anemia, hyperamylasemia, elevated creatine kinase, elevated transaminases and hypocomplementaemia [2]. Eosinophilia occurs in 14 percent to 80 percent of patients [5]. Because of varied and non-specific manifestations, CES closely resembles other systemic diseases such as endocarditis, polymyositis, periarteritis nodosa, and other vasculitides [6]. However, a skin biopsy revealing the typical features of CES differentiates it from other mimickers of the disease.
The mortality rate is high (81%) and is usually related to cardiac and renal complications [2]. CES should be considered in the differential diagnosis of patients presenting with sudden onset livedo reticularis, purpuric macules, or nodules with or without ulceration. The role of a dermatologist in making a diagnosis of CES is crucial because cutaneous manifestations are the most common physical findings.
References
1. Jucgla A, Moreso F, Muniesa C, Moreno A, Vidaller A. Cholesterol embolism: still an unrecognized entity with a high mortality rate. J Am Acad Dermatol. Nov 2006; 55(5): 786-93. [PubMed]2. Fine MJ, Kapoor W, Falanga V. Cholesterol crystal embolization: a review of 221 cases in the English literature. Angiology. 1987; 38: 769-784. [PubMed]
3. Falanga V, Fine MJ, Kapoor WN. The cutaneous manifestations of cholesterol crystal embolization. Arch Dermatol. 1998; 122: 1194-8. [PubMed]
4. Pennington M, Yeager J, Skelton H, Smith KJ. Cholesterol embolization syndrome: cutaneous histopathological features and the variable onset of symptoms in patients with different risk factors. Br J Dermatol. 2002; 146: 511-517. [PubMed]
5. Scolari F, Tardanico R, Zani R, Pola A, Viola BF, Movilli E, et al. Cholesterol crystal embolism: a recognizable cause of renal disease. Am J Kidney Dis. 2000; 36: 1089-109. [PubMed]
6. Richards AM, Eliot RS, Kanjuh VI, et al: Cholesterol embolism: A multiple-system disease masquerading as polyarteritis nodosa. Am J Cardiol. 1965; 15: 696-707. [PubMed]
© 2012 Dermatology Online Journal

