Primary cutaneous marginal zone lymphoma as a complication of radiation therapy: Case report and review
Published Web Location
https://doi.org/10.5070/D33bk973srMain Content
Primary cutaneous marginal zone lymphoma as a complication of radiation therapy: Case report and review
Anne-Laure Breton1, Nicolas Poulalhon1, Brigitte Balme2,3, Luc Thomas1, Stéphane Dalle1,3
Dermatology Online Journal 16 (12): 6
1. Service de dermatologie, Centre Hospitalier Lyon Sud, Pierre-Bénite, France2. Service d’anatomopathologie, Centre Hospitalier Lyon Sud, Pierre-Bénite, France
3. French Study Group on Cutaneous Lymphoma
Abstract
BACKGROUND: The occurrence of primary cutaneous B-cell lymphoma at the site of radiation therapy is exceptional. We report herein the case of a primary cutaneous marginal zone lymphoma arising at the site of radiotherapy for breast cancer. METHODS/RESULTS: A seventy-year-old woman was diagnosed in 2005 with an invasive ductal carcinoma of the left breast, which was treated with surgery, adjuvant chemotherapy, and radiation therapy. Three years later she developed several cutaneous nodules on her left breast, followed by similar lesions on her back. Histologic, immunohistochemistry, and molecular findings were consistent with the diagnosis of cutaneous marginal zone lymphoma. Physical examination was otherwise negative, as well as mammography, total body CT, bone marrow biopsy, and Borrelia serology. CONCLUSIONS: To our knowledge, this is the first published case of primary cutaneous marginal zone lymphoma occuring at the site of radiotherapy. Cutaneous surveillance is proposed from the first year after irradiation in order to detect new primary malignancies, including this rare cutaneous neoplasm.
Introduction
Primary cutaneous B-cell lymphomas (PCBLs) are rare cutaneous neoplasms. Low-grade PCBLs are divided into two distinct subtypes: primary cutaneous marginal zone lymphoma (PCMZL) and primary cutaneous follicle center lymphoma (PCFCL) [1, 2]. The latter has been exceptionally reported to occur in radiation fields [3, 4]. We report herein the original case of a PCMZL arising at the site of radiation therapy for breast cancer.
Methods and results
A seventy-year-old woman was diagnosed in March 2005 with an invasive ductal carcinoma of the left breast located at the junction of outer quadrants. TNM staging was pT1b, pN1a, M0. The patient was treated by lumpectomy, left axillary sentinel lymph node biopsy (positive), and completion lymph node dissection (negative). Six cycles of chemotherapy (5-fluorouracil, epirubicin, cyclophosphamide, and docetaxel) followed by radiotherapy (50 Gy on the left breast, supraclavicular, and medial mammary lymph node chains plus a 12-Gy boost on the tumoral bed) were administered as adjuvant therapy. The patient ended radiotherapy on November 2005 and was subsequently treated with hormone therapy. She is still in complete remission of breast cancer.
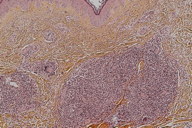
In March 2008, her physician noticed several asymptomatic skin lesions on her left breast. She was first referred to our unit in July 2008. Erythematous, firm nodules clustered on the upper outer quadrant of the left breast (Figure 1) and seven similar lesions scattered on the upper back were seen. Breast palpation and superficial lymph node areas were unremarkable. She was otherwise in good health.
Mammography and total body CT were normal. Human immunodeficiency virus, and Borrelia burgdorferi serologies were negative. Epstein-Barr virus serology was consistent with past immunization.
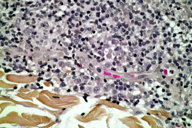
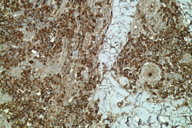
Histological examination showed a dermal nodular and diffuse lymphoid infiltrate separated from the epidermis by a grenz zone (Figure 2). Lymphoid cells were mostly small-sized, with slightly irregular nuclei devoid of nucleoli, relatively pale and abundant cytoplasms, and a strong plasmacytic differentiation. No large cell component was visible (Figure 3). Immunohistochemistry staining revealed 50 percent of CD20 and CD79-positive B-cells within nodules, expressing exclusively the kappa immunoglobulin light chain (Figure 4) and 50 percent of reactive CD3-positive T-cells. Bcl-6 and CD10 were negative. Ki67 was expressed in less than 10 percent of cells. Bcl-2 was positive only in T-cells. A B-cell clone was found by PCR for the FR1-JH and FR2-JH immunoglobulin receptor gene rearrangements. Bone marrow biopsy showed a reactive lymphoid infiltrate. The patient was then diagnosed with a PCMZL.
A 3-week treatment with amoxicillin did not improve the lesions. Complete remission was achieved after four weekly intravenous infusions of the anti-CD20 monoclonal antibody rituximab. Relapse occurred six months later showing two cutaneous nodules on her left breast and back. After six courses of rituximab plus oral chlorambucil, a partial response was obtained and a residual lesion of the trunk was excised.
Discussion
PCMZL is an infrequent low-grade B-cell lymphoma, most often of unknown etiology. Borrelia burgdorferi has been implicated in some cases [2]. Our patient’s case raises the hypothesis of a causal link between radiotherapy and PCMZL.
Skin exposure to ionizing radiation is known to increase the risk of sarcomas and carcinomas in various tissues including the skin [5, 6]. Single cases of primary extra-cutaneous lymphoma have also been reported [7, 8]. Cahan et al. defined criteria for radiation-induced malignancies: a history of previous irradiation, cancer arising at the irradiation field, histology different from initial neoplasm and more than five years between radiation and cancer [5].
Two cases of PCBL on an irradiation field have been already reported, corresponding in both cases to PCFCL [3, 4]. Only the case reported by Bachmayer et al. in 2007 included a detailed clinical and histological description [3]. In the latter case, a 74-year-old woman presented with a unique cutaneous nodule on the radiation site for breast cancer, which had been treated 8 years before [3]. Unlike Bachmayer’s observation, in our patient the lesions were multiple and were not located exclusively within the radiation field. Nevertheless, radiotherapy did presumably participate in lymphomagenesis, given that the first lesions were grouped on the left breast, within the irradiated area, and that patients with PCMZL are more likely to develop disseminated nodules than patients with PCFCL [2]. In addition, our case does not strictly meet Cahan’s criteria [5], because the time before the occurrence of PCMZL was three years. Yet, radio-induced sarcomas occuring less than five years at the site of radiation therapy for breast cancer have already been reported [9].
Mechanisms of radiation-induced lymphomagenesis include the induction of irreversible DNA mutations involving tumor suppressor genes, and more specifically altered interactions between p53 and PTEN pathways [10]. Moreover, chronic antigen stimulation induced by H. pylori and B. burgdorferi may play a role in gastric and skin marginal zone lymphomas, respectively [2]. Similarly, radiotherapy could unmask new epitopes in irradiated skin, which in turn could result in chronic stimulation of a reactive B-cell clone.
In our patient, the potential role of chemotherapy and/or hormonal therapy as co-carcinogenic factors may be considered. However, chemotherapy agents have never been associated with an increased incidence of solid tumors or lymphomas, whereas hormonal therapy as an adjuvant treatment of breast cancer is known to increase the risk of endometrial cancer only [6].
Conclusions
To the best of our knowledge, this is the first published case of PCMZL occurring on a radiation field. Therefore, cutaneous surveillance should be proposed beginning the first year after radiotherapy, in order to detect new primary malignancies that include carcinomas and also primary cutaneous lymphomas such as PCMZL.
References
1. Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, Ralfkiaer E, Chimenti S, Diaz-Perez JL, Duncan LM, Grange F, Harris NL, Kempf W, Kerl H, Kurrer M, Knobler R, Pimpinelli N, Sander C, Santucci M, Sterry W, Vermeer MH, Wechsler J, Whittaker S, Meijer CJ. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005 May 15;105(10):3768-85. [PubMed]2. Dalle S, Thomas L, Balme B, Dumontet C, Thieblemont C. Primary cutaneous marginal zone lymphoma. Crit Rev Oncol Hematol. 2010 Jun;74(3):156-62. [PubMed]
3. Bachmeyer C, Khosrotehrani K, Moguelet P, Aractingi S. Primary cutaneous follicular B-cell lymphoma arising at the site of radiotherapy for breast cancer. Br J Dermatol. 2007 Jan;156(1):198-9. [PubMed]
4. Maalej M, Frikha H, Kochbati L, Bouaouina N, Sellami D, Benna F, Gargouri W, Dhraief S, Nasr C, Daoud J, Hajji M, Fazaa B, Souissi R, Mokhtar I, Kamoun MR. Radio-induced malignancies of the scalp about 98 patients with 150 lesions and literature review. Cancer Radiother. 2004 Apr;8(2):81-7. [PubMed]
5. Cahan WG, Woodard HQ, et al. Sarcoma arising in irradiated bone; report of 11 cases. Cancer. 1948 May;1(1):3-29. [PubMed]
6. Schaapveld M, Visser O, Louwman MJ, de Vries EG, Willemse PH, Otter R, van der Graaf WT, Coebergh JW, van Leeuwen FE. Risk of new primary nonbreast cancers after breast cancer treatment: a Dutch population-based study. J Clin Oncol. 2008 Mar 10;26(8):1239-46. [PubMed]
7. Stein M, Haim N, Kuten A, Doron Y, Ben Arieh YT, Cohen Y. Primary brain lymphoma after X-ray irradiation to the scalp for tinea capitis in childhood. J Surg Oncol. 1992 Aug;50(4):270-3. [PubMed]
8. Yukiiri K, Mizushige K, Ueda T, Kohno M. Second primary cardiac B-cell lymphoma after radiation therapy and chemotherapy--a case report. Angiology. 2001 Aug;52(8):563-5. [PubMed]
9. Kirova YM, Vilcoq JR, Asselain B, Sastre-Garau X, Fourquet A. Radiation-induced sarcomas after radiotherapy for breast carcinoma: a large-scale single-institution review. Cancer. 2005 Aug 15;104(4):856-63. [PubMed]
10. Mao JH, Wu D, Perez-Losada J, Nagase H, DelRosario R, Balmain A. Genetic interactions between Pten and p53 in radiation-induced lymphoma development. Oncogene. 2003 Nov 20;22(52):8379-85. [PubMed]
© 2010 Dermatology Online Journal