Localized and persistent erythema nodosum leprosum - a rare variant?
Published Web Location
https://doi.org/10.5070/D32xv335d1Main Content
Localized and persistent erythema nodosum leprosum - a rare variant?
Smitha Prabhu1, Raghavendra Rao1, Sripathi H1, Laxmi Rao2, Ridhi Singh1
Dermatology Online Journal 14 (3): 16
1. Department of Skin & STD, Kasturba Medical College, Manipal, Karnataka, India. smithaprabhu@msn.com, drsmithaprabhu@yahoo.com2. Department of Pathology, Kasturba Medical College, Manipal, Karnataka, India
Abstract
Erythema nodosum leprosum (ENL) or Type-2 Lepra reaction is a manifestation of type III hypersensitivity response and usually occurs in certain cases of lepromatous and borderline lepromatous leprosy. It is usually generalized and evanescent, and responds well to oral corticosteroid therapy. Here we report an unusual case of persistent and localized ENL in a 19-year-old girl, which could be diagnosed with the aid of skin biopsy and histopathological examination.
Introduction
Erythema nodosum leprosum is an acute inflammatory reaction seen in a patient with lepromatous leprosy or occasionally, with borderline lepromatous leprosy. It is a manifestation of Type-2 lepra reaction, which is in turn a Coomb and Gell Type III hypersensitivity reaction. This condition is usually associated with multidrug therapy (MDT), especially in patients with high Bacteriological Index. It may be seen in untreated patients.
Case Report
A 19-year-old girl presented to our department with erythematous painful papules and nodules on the posterolateral aspects of both thighs, more on the left side, of 6 weeks duration. She also had mild fever for the past 1 week, along with occurrence of a few new nodules on her face and upper extremities for 3-5 days. She had been treated in the past for borderline lepromatous leprosy, and had a history of recurrent Type-2 lepra reaction for the past year.
Her leprosy was detected 3 years back in a peripheral government hospital, when she developed pedal edema and a non-healing ulcer of right leg. On examination, multiple hypopigmented patches were detected on the back and forearms with glove and stocking hypoaesthesia. Biopsy of a representative lesion was consistent with borderline lepromatous leprosy. She was started on the multibacillary 3-drug regimen and was released from treatment after completion of 2 years. Within a couple of month's time, she presented to us with erythematous tender nodules over extremities and trunk, associated with mild fever. Slit skin smear examination for acid fast bacilli from representative sites revealed a Bacteriological Index of 3+, Morphological Index being zero. She was started on Clofazimine 100 mg twice daily and prednisolone 30 mg daily, which helped in controlling the reaction. She was irregular in follow-up and was not compliant with treatment.
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Grouped papules and nodules on posterolateral aspect of right thigh and buttock Figure 2. Ichthyotic patches on both legs | |
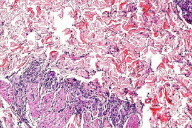
On current examination, she had a few scattered erythematous tender nodules and papules varying from 0.5-1 cm in diameter over face and extremities, along with grouped erythematous, tender papules and nodules over the posterolateral aspect of both thighs extending to the buttocks.
Multiple ill-defined ichthyotic patches were seen over limbs and back. A few atrophic scars were present over the arms and shins. She also had painful swelling of fingers. Bilateral ulnar and radial cutaneous nerves were thickened and the right ulnar nerve was tender. Routine investigations done included fasting and post-prandial blood sugar levels, renal and liver function tests, early morning serum cortisol, and complete blood count; these were all within normal limits, except for a low hemoglobin level of 10 mg percent. In view of the persistent grouped lesions of the postero-lateral aspect of the left thigh, which did not conform to the morphology of ENL, and because she was already on oral steroids and high dose clofazimine, we favored a diagnosis of insect bite reaction. A biopsy was taken from the lesion for histopathological examination which revealed the following features.
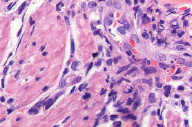
A thinned out epidermis, with dermis showing compact cellular aggregates of foamy macrophages in periadnexal and perineural locations with infiltration of arrector pilori, surrounded by a lymphocytic infiltrate. Dermal vessels were edematous and infiltrated with neutrophils. A few neutrophils and nuclear debris were seen in the dermis. Fite stain was positive in foamy macrophages, favoring a diagnosis of borderline lepromatous leprosy with Type-2 lepra reaction.
She was started on oral prednisolone 1mg/kg body weight, i.e., 40 mg daily in a single morning dose after breakfast, along with oral pantoprazole 40 mg on an empty stomach. Indomethacin 25 mg bid po and oral multivitamin tablets were also given. She responded well within a week's period, after which prednisolone was tapered by 5 mg per week and finally stopped after 8 weeks. Clofazimine was not restarted as the patient was excessively concerned about her darkening skin color. If she had not shown a good response to oral steroids, we would have started her on clofazimine 100 mg twice daily or even thalidomide 100 mg tid, after getting a written consent after careful explanation regarding its side effects, especially its teratogenic potential. She was kept on monthly follow-up and has not developed any new episodes of ENL for the past one year. As the leprosy infection was adequately treated, we have not re-started her on anti-leprosy treatment.
Discussion
Leprosy is a chronic, slowly progressive granulomatous infection caused by the bacillus, Mycobacterium leprae. Reactions are acute episodes superimposed on the chronic course of leprosy. Type-1 lepra reaction is a delayed type hypersensitivity reaction occurring in borderline leprosy cases. Type-2 lepra reaction, the skin lesions of which are termed erythema nodosum leprosum (ENL), is an antigen antibody-mediated immune complex reaction, usually seen in lepromatous or sometimes borderline lepromatous leprosy. It usually occurs later during the course of treatment and in long-standing untreated cases [1]. Usually 15-50 percent of lepromatous leprosy patients develop ENL reactions within the first year of therapy. More than 50 percent of lepromatous leprosy patients and 25 percent of borderline lepromatous leprosy patients used to experience ENL reactions in the pre MDT era [2]. However, ENL reactions may occur later during therapy or even after discontinuation of therapy. There are certain known triggers of ENL which include stress, pregnancy, lactation, concurrent illness, and medication. There is a sudden occurrence of crops of pink to reddish tender nodules or plaques, which occasionally become vesicular, pustular, bullous or gangrenous. Necrotic and erythema multi-forme like variants have also been described in the literature [3]. The pre-existing lesions do not undergo any change. It may be associated with peripheral edema, iritis, iridocyclitis, epididymoorchitis, arthritis, muscle and bone pain and proteinuria secondary to glomerulonephritis. Mild ENL is intermittent and evanescent, but severe ENL may persist for years. Histologically it is characterized by an inflammatory cell infiltrate, composed predominantly of a large number of neutrophils, along with acute vasculitis in the dermis and adjacent subcutis.
Immunosuppressants, particularly oral corticosteroids are the mainstay of treatment in moderate to severe cases, as these provide the most rapid control of the lesions, although thalidomide is considered to be the drug of choice. Analgesics and anti-inflammatory drugs are usually co-prescribed for alleviation of pain and inflammation, but may be the sole agents used in the treatment of mild cases [4]. Although antimonials are particularly effective in alleviating bone and joint pain, these are not used frequently nowadays due to their potent side-effects. The anti-leprosy drug clofazimine, in higher doses, is indicated in patients with persistent ENL who cannot use thalidomide and who cannot be weaned off corticosteroids successfully.
There are a few case reports of unusual variants of ENL reported so far in the literature. Erythema nodosum lerposum clinically presenting as urticarial vasculitis in a patient who was then diagnosed to have lepromatous leprosy has been reported by Funk W K [5]. Dave et al have reported a case of pustular ENL occurring in a patient after switching from MB MDT to ofloxacin-aided MDT [6]. Galvez et al reported the atypical evolution of borderline leprosy as well as a Type-2 lepra reaction predominantly involving multiple nerves rather than skin [7]. Sethuraman et al have reported a severe bullous variety of ENL in a 35-year-old man, which could be controlled only by IV hydrocortisone [3]. A bullous-type reaction mimicking pemphigus in a lepromatous leprosy patient has been described by Petro from India. In this patient other constitutional features and neuritis were absent; histopathological examination from the lesion was not done [8]. An episode of ENL involving the orbit, causing vasculitis of the orbital apex, leading to orbital apex syndrome and ocular ischemia in a lepromatous leprosy patient with recurrent ENL has been reported by Dhaliwal et al [9]. Kou et al have reported a male with underlying lepromatous leprosy presenting with an atypical reactional state simulating Sweet syndrome. Sweet syndrome has been recognized as a variant of ENL for which administration of high dose systemic corticosteroids has been beneficial [10].
Conclusion
Although various rare and atypical variants of ENL have been described in the literature, this persistent and localized variant has never been reported to the best of our knowledge. Our patient had a documented history of recurrent ENL reactions while on treatment as well as after release from treatment. Maybe, her non-compliance to oral steroids and clofazimine did contribute to the frequent recurrences of the reaction. She showed a good response to supervised intake of oral prednisolone 40 mg/day under hospitalization and was discharged within a week with tapering doses of corticosteroids and other adjuvants. Her follow-up period of one year has been uneventful.
References
1. Meyerson MS. Erythema nodosum leprosum. Int J Dermatol 1996; 35: 389-392. PubMed PubMed2. Pflatzgraff RE, Bryceson A. Clinical leprosy. In: Hastings RC, Opromolla DVA, ed. Leprosy. London: Churchill Livingstone, 1985:165-171.
3. Sethuraman G, Jeevan D, Srinivas CR, Ramu G. Bullous erythema nodosum leprosum (bullous type II reaction). Int J Dermatol 2002;41:362-364.
4. The management of erythema nodosum leprosum. ILEP Technical Bulletin. Issue No. 9, May 1996.
5. Funk W K.Lepromatous leprosy and erythema nodosum. Hongkong dermatology and venereology bulletin 2001;28-30.
6. Dave S, Thappa DM, Nove AV, Jayanthi S. A rare variant of erythema nodosum leprosum: a case report. Dermatol Online Journal 9(5):11.
7. Galvez J, Lopez-Dominguez JM, Navarro A, et al. Patient with Hansen disease and lepromatous reaction with predominant neural involvement. Neurologia 1998;13:41-44. (Pubmed abstract of Spanish article) PubMed
8. Petro TS. Bullous type of reaction mimicking pemphigus in lepromatous leprosy. Indian J Lepr 1996;68:179-181.
9. Dhaliwal U, Mohanty S, Bhattacharya S N. Erythema nodosum leprosum and orbital involvement. Int J Lepr and other Mycobacterial diseases 2003:71:10-13.
10. Kou TT, Chan HL. Severe reactional state in lepromatous leprosy simulating Sweet's syndrome. Int J Dermatol 1987;26:518-520.
© 2008 Dermatology Online Journal