Severe 20-nail psoriasis successfully treated by low dose methotrexate
Published Web Location
https://doi.org/10.5070/D32xf4v4pwMain Content
Severe 20-nail psoriasis successfully treated by low dose methotrexate
Julia Yu-Yun Lee MD
Dermatology Online Journal 15 (11): 8
Professor, Department of Dermatology, National Cheng Kung University, College of Medicine and University Hospital, Tainan,
Taiwan. yylee@mail.ncku.edu.twAbstract
Severe involvement of the nail matrix can lead to extensive dystrophic changes of the nail plate. Topical or intralesional corticosteroids, photochemotherapy, oral retinoids, and methotrexate (MTX) are among the therapies used. Treatment of severe psoriatic nail disease is often unsatisfactory. We report a case of severe psoriatic nail dystrophy involving all 20 nails successfully treated by low dose MTX. A previously healthy 11-year-old girl presented with painful deformity involving all 20 nails that developed over a one-month period. Examination revealed geographic and fissured tongue, as well as severe nail dystrophy of all 20 nails characterized by erythematous swelling of the nail folds, yellowish discoloration of nail plates with pitting, severe crumbling and destruction, transverse depressions, prominent oil spots, and swelling of proximal nail. Topical clobetasol propionate and calcipotriol were tried first but the nail dystrophy continued to progress. Low dose of MTX (5 mg per week) was initiated. The response was fairly satisfactory with emergence of normal plate proximally as early as 4 weeks; complete resolution of the severe nail dystrophy was achieved after 9 and 13 months of MTX therapy for fingers and toes, respectively. The present case illustrates that weekly low dose oral MTX may be a good treatment option for severe psoriatic nail dystrophy in patients without other contraindications for MTX therapy.
Introduction
Various parts of the nail unit are affected in 10-50 percent of patients with psoriasis [1, 2, 3]. In less than 5 percent of the time the nails may be involved without obvious skin lesions [4]. Psoriatic nail disease manifests as pitting, "oil spots" or "oil drop" sign, onycholysis, subungual hyperkeratosis (onychoauxis), splinter hemorrhage, onychorrhexis, Beau's lines, and onychomedesis, depending on the specific structure of the nail unit affected and severity of the involvement [4]. Pustular psoriasis of the nail units or acrodermatitis continua starts as pustules under the nail and leads to extensive destruction of the plate [3].
The pathology of psoriatic nails is similar to that observed in the skin with parakeratosis, acanthosis, and inflammatory changes [3, 5]. Nail pitting is caused by intermittent parakeratosis of the proximal matrix. The light-brown or yellowish red discoloration of the "oil drop" sign, which is virtually pathognomonic for psoriasis [2], reflects deposition of glycoproteins in the nail bed with onycholysis. Onycholysis and subungual hyperkeratosis is a consequence of abnormal keratinization of the nail bed. Severe involvement of the nail matrix can lead to extensive dystrophic changes of the nail plate. Treatment of severe psoriatic nail is often unsatisfactory. We report a case of severe 20-nail psoriasis successfully treated by low dose methotrexate (MTX).
Case synopsis
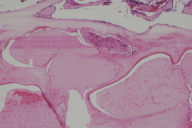
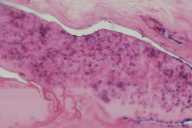
A previously healthy 11-year-old girl first presented to our clinic in September 2006 with painful deformity of all 20 nails. The mother reported that the disease began one month previously with pus-like fluid expressed from underneath the nail. The nail changes had a sudden onset without a preceding event including infection, fever, sore throat, arthralgia or medication, but a small pustule had been noted on the abdomen. Examination revealed severe nail dystrophy of all 20 nails characterized by erythematous swelling of the nail folds, yellowish discoloration of the plates with pitting, prominent oil spots, severe crumbling and destruction, transverse depressions, and swelling of proximal nail (Figs. 1A & 1B). The patient had geographic and fissured tongue. Her mother had geographic tongue.
A tentative diagnosis of acrodermatitis continua involving all 20 nails with severe nail dystrophy was made. HLA-B27 was negative. Pathologic examination of the distal nail plates revealed marked thickening of the nail plates with intraonychial vesiculopustules and subungual parakeratosis containing neutrophils and plasma globules. The changes were consistent with psoriasis.
Treatment with clobetasol proprionate ointment 0.05 percent under occlusion was initiated. Calcipotriol solution 0.005 percent was added 4 weeks later. The disease continued to progress after 7 weeks of treatment and the nail became more thickened (Fig. 1C & 1D). Because of the poor response and the severe disfigurement, the mother and the patient consented to oral MTX therapy. Her body weight was 31 kg. MTX 5 mg weekly in two divided doses 12 hours apart was initiated. Complete blood cell counts and liver function tests were monitored periodically. Normal-appearing nail began to emerge proximally a month later. After 9 months of MTX therapy, the nail dystrophy was markedly improved with residual pitting, ridging, discoloration and thickening. The fingernails and toenails looked normal after 9 and 13 months of MTX therapy, respectively.
MTX was continued until January 2008 for a total of 15 months. A follow-up photo in February 2008 revealed residual thickening of the distal end of big toenails (Figs. 5C & 5D). In September 2008, the patient returned to the clinic with recurrence involving the proximal finger and toenails. Reinstitution of MTX 7.5 mg per week halted the progression of the nail changes of fingers in one month and of toes in two months. The fingernails normalized in 6 months. The toenails took a longer time to recover; as of June 2009, only the distal edges of the toe nails remained thickened. The dose of MTX was tapered to 7.5 mg per 10 days. One month later, the proximal nail folds of the fingers appeared swollen. To prevent a potential recurrence, the dose of MTX was increased to 7.5 mg per week. The MTX therapy was well tolerated without side effects.
Nail psoriasis is difficult to treat and there is no consistently effective treatment. Moreover, the treatment response is slow and relapse is common [6, 7]. Topical or intralesional corticosteroids, photochemotherapy, oral retinoids, and MTX are among the therapies used [7]. Oral retinoids were effective in 6 of 12 patients [8]. Feliciani et al. [9] reported improvement in 79 percent of the cases with psoriatic nail using systemic cyclosporine 3.5 mg/kg/d combined with topical calcipotriol twice daily for 3 months. MTX therapy may result in good improvement in the nail, but is usually not recommended except in severe pustular psoriasis or extreme cases of nail involvement [10].
In the present case, the disease first manifested as subungual pustules that proceeded to severe nail dystrophy with extensive destruction of the plates of all digits. Except for geographic tongue, our patient's psoriasis was limited to the nails. Because of the severity and the extent of the nail involvement and the young age of the patient, intralesional corticosteroid injection was rejected as being too painful to be acceptable. Topical clobetasol propionate and calcipotriol were tried first with no avail. The effect of low dose of MTX (5 mg per week) was proven to be satisfactory with emergence of normal plate proximally as early as 4 weeks. Complete resolution of the severe nail dystrophy was achieved after 9 and 13 months of MTX therapy for fingers and toes, respectively. There was recurrence of nail psoriasis of all 20 nails 8 months after MTX was discontinued. The progression of the nail changes was quickly halted and the fingernails returned to normal in 6 months after reinstatement of MTX. It is peculiar that both the first occurrence and the recurrence of the nail psoriasis in our patient happened in the summer. In view of this history, we are concerned that the newly developed swelling of the proximal nail folds in July of this year (2009) may be the herald sign of a potential recurrence.
In summary, we presented a case of severe nail psoriasis involving all 20 nails; it was successfully treated by weekly low dose MTX in its first attack and the subsequent recurrence 2 years later. The present case illustrates that weekly low dose oral MTX may be a good treatment option for severe psoriatic nail dystrophy for patients who have no other contraindication for MTX therapy.
References
1. Zaias N. Psoriasis of the nail: A clinical pathological study. Arch Dermatol 1969;99:567-79. [PubMed]2. Scher RK. Psoriasis of the nail. Dermatol Clin 1985;3:387-94. [PubMed]
3. Baden HP. Nail abnormalities associated with cutaneous diseases. In: Disease of the hair and nails. Chicago: Year Book Med Publishers Inc, 1987;48-51.
4. Basuk PJ, Scher RK, Ricci AR. Dermatologic diseases of the nail unit. In: Nails: Therapy, diagnosis, surgery (Scher RK, Daniel CR III, eds). Philadelphia: W.B. Saunders Co,1990;127 & 133.
5. Lewin K, DeWit S, Ferrington RA. Pathology of the finger nail in psoriasis. A clinicopathological study. Br J Dermatol 1972;86:555-63. [PubMed]
6. de Berker D. Management of nail psoriasis. Clin Exp Dermatol 2000;25:357-62. [PubMed]
7. Farber EM, Nall L. Nail psoriasis. Cutis 1992;50:174-8. [PubMed]
8. Piraccini BM, Totsi A, Iorizzo M, Misciali C. Pustular psoriasis of the nails: treatment and long-term follow-up of 46 patients. Br J Dermatol 2001;144:1000-5. [PubMed]
9. Feliciani C, Zampetti A, Forleo P, et al. Nail psoriasis; comined therapy with systemic cyclosporin and topical calcipotril. J Cutan Med Surg 2004;8:122-5. [PubMed]
10. Roenigk HH, Auerbach R, Maibach HI, et al. Methotrexate guidelines-revised. J Am Acad Dermatol 1982;6:145-55. [PubMed]
© 2009 Dermatology Online Journal