Systemic drug-related intertriginous and flexural exanthema (SDRIFE)
Published Web Location
https://doi.org/10.5070/D32ws5h2s0Main Content
Systemic drug-related intertriginous and flexural exanthema (SDRIFE)
Sarina B Elmariah MD PhD, Wang Cheung MD, Nadia Wang MD, Hideko Kamino MD, Miriam K Pomeranz MD
Dermatology Online Journal 15 (8): 3
Department of Dermatology, New York UniversityAbstract
A 72-year-old man with a history of metastatic melanoma presented with a two-day history of erythematous and edematous plaques, with scattered bullae on the neck, chest, axillae, and inguinal and gluteal folds, which began five days after infusion of an experimental drug. The clinical and histopathologic findings were consistent with systemic drug-related intertriginous and flexural exanthema (SDRIFE), which is an uncommon drug reaction that results in symmetric erythema that affects the buttocks, groin, and/or thighs as well other flexural folds. The clinical manifestations of SDRIFE are highly characteristic and include distinctive primary cutaneous lesions with a specific distribution and course; however, heterogeneity exists with respect to histopathologic features, skin test results, and in vitro investigations. The exact mechanism of SDRIFE remains unknown but is thought to result from a type IV delayed hypersensitivity immune response. Treatment is symptomatic and includes topical or oral glucocorticoids.
 |  |
| Figure 1 | Figure 2 |
|---|---|
History
A 72-year-old man was hospitalized at New York University Langone Medical Center in August, 2008, with a two-day history of subjective fevers and an erythematous eruption on his neck, chest, antecubital fossae, axillae, and inguinal and gluteal folds. He had received his first infusion of CR011-vcMMAE, which is an experimental monoclonal antibody-Auristatin E conjugate, for treatment of metastatic melanoma seven days prior to the onset of his symptoms. Over the course of 18 hours, the patient developed intense pruritus, erythema, and bullae in the affected areas. He denied skin tenderness or involvement of the oral, ocular, genital, or perianal skin. He was evaluated by the Dermatology Service during his hospitalization, and biopsy specimens were obtained from the left axilla and left inguinal fold. The patient was treated with topical glucocorticoids and antihistamines, with partial resolution of the eruption over two to three weeks. He subsequently has received infusions of CR011-vcMMAE with recurrence of the eruption, which was attenuated by the use of methylprednisolone and anti-histamines administered before and after infusions.
Medical history includes hypertension and metastatic melanoma, which was initially diagnosed with primary involvement of the right great toe in 2003. Metastases to the right leg and inguinal lymph nodes were noted in 2007. He received systemic chemotherapy in 2007, with subsequent isolated limb perfusion with melphalan in April, 2008. Past surgical history includes amputation of the right great toe in 2003 and radical lymph node dissection in 2008. His current medications include valsartan, metoprolol, oxycodone and acetaminophen, and a multivitamin. He has an allergy to penicillin, which has caused an eruption in the past. He has no known family history of skin disease.
Physical examination
On the inferior portion of the neck and upper chest were ill-defined, erythematous patches. On the right antecubital fossa, axillae, proximal thighs, inguinal folds, buttocks, and gluteal folds, erythematous, edematous plaques with scattered, tense vesicles and bullae were present. On the right leg, multiple, blue and black crusted nodules were present, each of which was surrounded by a well-circumscribed rim of erythema.
Laboratory data
A complete blood count, comprehensive metabolic panel, and a hepatic function panel were normal, except for a mild elevation in amylase at 132 Units/L. Blood and urine cultures resulted in no growth. A Tzanck smear and viral and bacterial cultures obtained from an intact bulla were negative. A chest radiograph showed no acute cardiopulmonary disease.
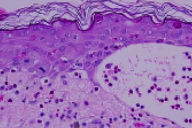
Histopathology
There is a subepidermal bulla due to basal vacuolar alteration. In the adjacent and overlying epidermis, there are necrotic keratinocytes, epidermal dysmaturation, and increased mitotic figures. The cornified layer is a basket-weave pattern. There also is an infiltrate of lymphocytes, neutrophils, and numerous eosinophils in the dermis and in the bullous cavity.
Comment
Systemic drug-related intertriginous and flexural exanthema (SDRIFE) is an uncommon, yet distinct, cutaneous reaction that occurs after the systemic administration of drug-related allergens [1]. The term "baboon syndrome" was originally introduced by Andersen and colleagues in 1984 to describe sharply-demarcated erythema of the buttocks and inner thighs that was observed in three patients who were exposed to mercury, nickel, and ampicillin. This condition resembled the red gluteal region of baboons [2]. To date, over 100 cases of similar eruptions have been described under several names, which include eczema rubrum, systemically induced allergic contact dermatitis, systemic contact dermatitis, paraptic eczema, or drug-induced intertrigo [3]. In 2004, the acronym SDRIFE was proposed to encompass the specific clinical pattern noted in these reactions, regardless of known prior sensitization. This condition is characterized by five clinical criteria: occurrence after exposure to systemic drugs, sharply-demarcated erythema of the buttocks and/or V-shaped erythema of the thighs, involvement of at least one other flexural fold, symmetry, and the absence of systemic symptoms [1, 3]. Lesional skin may have papules, pustules, vesicles, and bullae. Involvement of the palms, soles, face, or mucosae is rare.
Systemic drug-related intertriginous and flexural exanthema may affect patients of any age, with case reports of individuals ranging from 18 months to 84 years [3]. Both genders are affected with a slight male predominance. The onset of flexural erythema usually begins hours to days after systemic exposure to the inciting agent. Systemic drug-related intertriginous and flexural exanthema is most commonly observed after exposure to beta-lactam antibiotics, such as penicillins and cephalosporins, with amoxicillin being implicated in the majority of cases [1, 2, 3, 4]. Systemic drug-related intertriginous and flexural exanthema also has been reported after the administration of mercury, nickel, heparin, allopurinol, erythromycin, hydroxyurea, oxycodone, pseudoephedrine, aminophylline, terbutaline, barium sulfate, iodinated radiocontrast media, intravenous immunoglobulin, and cetuximab. To our knowledge, this is the first case of SDRIFE reported secondary to CR011-vcMMAE, which is a humanized monoclonal antibody against glycoprotein NMB, a transmembrane tumor-associated protein expressed on melanoma cells, that is conjugated to the cytoxin monoethylauristatin. As in the case of SDRIFE triggered by other biologic agents that contain immunoglobulins, the eruption occurred in our patient in the absence of a known prior sensitizing exposure.
Whereas the exact pathogenetic mechanism underlying SDRIFE is not clear, it is thought to involve a type IV delayed-hypersensitivity immune response. The specific sensitizing agent is frequently not known or is undocumented. Moreover, negative patch or prick tests occur in approximately one-third to one-half of the patients [3, 6, 7, 8]. Nonetheless, many patients have delayed reactions to nickel, mercury derivatives, or the causative antibiotic on patch testing [4, 6]. A role for a type IV delayed immune response also is supported by immunohistochemical evidence for CD4+ T cell infiltration and increased endothelial and keratinocyte expression of CD62P, which allows for T-cell recruitment to the skin [6].
Systemic drug-related intertriginous and flexural exanthema is self-limited, and treatment is directed toward symptomatic relief. Medium-to-high potency topical or systemic glucocorticoids may hasten recovery. Avoidance of systemic administration of precipitating drugs or allergens is recommended.
References
1. Häusermann P, et al. SDRIFE - another acronym for a distinct cutaneous drug exanthema: do we really need it? Dermatology 2007; 214: 1 [PubMed]2. Andersen KE, et al. The baboon syndrome: systemically-induced allergic contact dermatitis. Contact Derm 1984; 10: 97 [PubMed]
3. Hausermann P, et al. Baboon syndrome resulting from systemic drugs: is there strife between SDRIFE and allergic contact dermatitis syndrome? Contact Derm 2004; 51: 297 [PubMed]
4. Lerch M, Bircher AJ. Systemically induced allergic exanthema from mercury. Contact Derm 2004; 50: 349 [PubMed]
5. Arnold AW, et al. Recurrent flexural exanthema (SDRIFE or baboon syndrome) after administration of two different iodinated radio contrast media. Dermatology 2007; 214: 89 [PubMed]
6. Barbaud A, et al. A baboon syndrome induced by intravenous human immunoglobulins: report of a case and immunological analysis. Dermatology 1999; 199: 258 [PubMed]
7. Sans V, et al. Baboon syndrome induced by cetuximab. Arch Dermatol 2008; 144: 272 [PubMed]
8. Barbaud A, et al. Tests cutanés dans l'investigation des toxidermies: de la physiopathologie aux résultats des investigations. Therapie 2002; 57: 258 [PubMed]
9. Handisurya A, et al. SDRIFE (baboon syndrome) induced by penicillin. Clin Exp Dermatol 2008; advanced e publication [PubMed]
10. Wolf R, et al. Intertriginous drug eruption. Acta Derm Venereol 1992; 72: 441 [PubMed]
11. Garcia-Bravo B, et al. Systemic contact dermatitis due to deflazacort. Contact Derm 2000; 43: 359 [PubMed]
© 2009 Dermatology Online Journal

