CD30+, large T-cell lymphoma: Diagnostic distinction and management
Published Web Location
https://doi.org/10.5070/D32tz1w7p0Main Content
CD30+, large T-cell lymphoma: Diagnostic distinction and management
Eric C Parlette MD1, Camille A Tabor MD2
Dermatology Online Journal 12 (6): 8
1. Uniformed Services University of Health Sciences, Department of Dermatology, US Naval Hospital, Okinawa, Japan. ecparlette@yahoo.com2.
USS Boxer, LHD-4, San Diego, CAAbstract
Cutaneous T-cell lymphoma (CTCL) has a variable presentation and comprises a broad diagnostic group. Histologic and immunophenotypic confirmation is needed to establish a precise diagnosis. Once the categorization is determined, prognosis and therapeutic algorithms unfold. Primary cutaneous, CD-30+, anaplastic, large T-cell lymphoma represents an indolent form of CTCL that often spontaneously involutes.
Cutaneous T-cell lymphoma (CTCL) is a broad diagnosis encompassing a spectrum of disease. The European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project recognizes mycosis fungoides (MF), cutaneous CD30-positive large-cell lymphoma, and lymphomatoid papulosis as CTCLs with indolent clinical behavior [1]. Clinical presentation and immunohistochemistry together are needed to determine the subtype of CTCL, which guides proper management.
Clinical synopsis
 |
| Figure 1 |
|---|
| Figure 1. Left hip with ulcerated, escharotic plaque with dermal infiltration. |
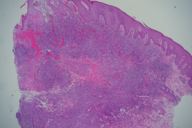
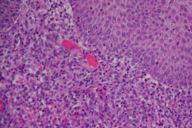
A 66-year-old woman with no significant past medical history presented with a 6-week history of a 3.5-cm, ulcerated, escharotic plaque with rolled borders on her left hip (Fig. 1). No lymphadenopathy was appreciated. Punch biopsy showed a dense, diffuse, top-heavy infiltrate (Fig. 2a) of highly mitotically active lymphoid cells with irregular, large nuclei (Fig. 2b). Deep vessels had a perivascular infiltrate of the lesional cells. Focal necrosis was found in areas of maximum infiltrate. Immunohistochemistry showed positivity for CD3, CD4, CD5, CD8, CD30 (Fig. 3), CD43, CD45RO, and negativity for CD15, CD20, LCA, EMA, ALK1. Correlating histology with the clinical picture allowed the diagnosis to be made: cutaneous malignant lymphoma, anaplastic large, T-cell type. Complete blood count with smear was normal.
 |
| Figure 3 |
|---|
| Figure 3. Dense, "top-heavy" infiltrate with diffuse CD30-positivity. |
The patient returned 26 days following her initial visit with reduction of the left hip plaque to 2.5 cm but with development of a new 1-cm, violaceous nodule on the right thigh. Clobetasol ointment twice a day was prescribed for the right thigh nodule. No treatment was initiated as this time for the left hip plaque given its rapid involution. Again, no lymphadenopathy was noted. Eleven days later, the left hip lesion had completely resolved leaving a hypopigmented, atrophic scar. The right thigh nodule had involuted to a small, 5-mm, faintly violaceous macule.
Hematology-oncology assessment was arranged. Evaluation was unremarkable, including a normal PET scan. However, despite clinical resolution, the diagnosis of anaplastic large cell lymphoma prompted hematology/oncology to recommend conservative treatment with local radiation therapy. The patient completed the treatment uneventfully. The patient continues to be disease free at 2-year followup with no further treatment.
Discussion
Primary cutaneous CD30-positive large-cell lymphoma represents about 10 percent of all cases of CTCL [1]. Primary cutaneous CD30-positive large cell lymphoma is defined according to the following criteria [2, 3]:
- no clinical evidence of lymphomatoid papulosis
- no previous or concurrent lymphomatoid papulosis, mycosis fungoides, or other (cutaneous) lymphoma
- no extracutaneous localization at presentation
- predominance (>75 %) of large clusters of CD30-positive blast cells in the initial skin biopsy
CD30+, cutaneous large T-cell lymphoma and lymphomatoid papulosis (LyP) are considered by some to be within the same spectrum of low-grade, cutaneous, anaplastic, large-cell lymphomas (ALCL). Clinical distinction can be argued between the two. Because both portray similar histology with atypical CD30+ T-cells, clinical appearance is stressed by EORTC to distinguish between the diagnoses and to delineate treatment.
CD30+ cutaneous T-cell lymphoma usually presents in adults from 45 to 60 years of age, being more frequent in males. It presents as one to several localized nodules or tumors with ulceration. Twenty percent of cases are multifocal. Plaques are greater than 1 cm in most cases (77 %) [4]. Trunk and extremities are most commonly involved. Presentation may be variable, being mistaken for other skin disorders such as adult-onset eczema, pyoderma gangrenosum, morphea, localized scleroderma, or squamous cell carcinoma [5]. Consequently, appropriate diagnosis may be delayed.
Lymphomatoid papulosis is a chronic disease that is widespread with recurring crops of numerous papules, nodules and plaques. Lesions evolve and may necrose and ulcerate. The onset of LyP is earlier, typically the third or fourth decade, although it rarely presents in children. Females are more commonly affected. There is an increased incidence of associated lymphoproliferative disorders with LyP, such as mycosis fungoides and Hodgkin lymphoma. Reportedly, 5-10 percent may evolve to malignant lymphoma [6]. Spontaneous resolution with episodic recurrence is common.
Despite the anaplastic nature, primary cutaneous, CD30+, anaplastic large T-cell lymphomas are no more aggressive than non-anaplastic type of CD30+ T-cell lymphomas. The EORTC combines these two histologically distinct, but clinically similar, cutaneous lymphomas into the diagnosis of CD30+ large T-cell lymphoma [1]. Histological examination shows diffuse, non-epidermotropic infiltrates with cohesive sheets of large CD30-positive tumor cells, oval or irregularly shaped nuclei, prominent eosinophilic nucleoli, and abundant cytoplasm. Additional common features are epidermal ulceration (63 %), prominent vascular proliferation (60 %), pseudoepitheliomatous hyperplasia (55 %), tumor necrosis (55 %), and vascular infiltration by neoplastic cells (44 %). [4] Occasionally (20-25%), Reed-Sternberg-like pleomorphic or immunoblastic cells are present. [7] The mitotic index is high. Reactive lymphocytes and plasma cells rarely present at the periphery.
Immunohistochemistry is essential in determination of CTCL subtypes and in the differentiation between primary and secondary disease. A predominance of greater than 75 percent CD30+ T-cells must be present for diagnosis as CD30+ large T-cell lymphoma. Neoplastic cells express an activated CD4-positive T-cell phenotype with variable loss of CD2, CD3, and CD5 [7].
CD30+ cells may be positive in other CTCLs, especially tumor-stage MF and subtypes of LyP. EORTC subclassifies LyP into histological subtypes, A, B, and C. Types A and C both express CD30+ cells. Histologically, Type C may resemble CD30+ large T-cell lymphoma [6].
Once clinical appearance, histology, and immunohistochemistry support the diagnosis of CD30+ large T-cell lymphoma, a thorough examination with attention to skin, lymph nodes, spleen, and liver is necessary. Chest radiography, computed tomography of abdomen and pelvis, bone marrow biopsy, lymph node analysis, and complete blood count with smears can further assist in indentification and staging of secondary cutaneous systemic lymphoma. Multidisciplinary care is optimal. Twenty-five percent of CD30+ CTCLs have lymph node involvement at presentation and 12 percent are secondary cutaneous lesions [3, 8].
A multitude of therapies are utilized for the spectrum of cutaneous T-cell lymphomas. Treatment varies with the diagnostic category and scope of disease. Partial or complete remission occurs with 42 percent of CD30+ CTCLs [8]. Relapse occurs in approximately 40 percent of patients despite treatment [8]. Extracutaneous disease occurs in 10-25 percent of CD30+ lymphomas despite treatment [2, 8]. Local radiotherapy or surgical excision is effective for one to several CTCL plaques, nodules, or tumors. If the neoplasm relapses, spontaneous resolution may occur over a period of weeks, otherwise treatment may be repeated. Treatment of multifocal disease is challenging. Subcutaneous or oral methotrexate may reduce generalized disease but does not prevent progression to more aggressive lymphoma [9]. Chemotherapy should be reserved for patients with more generalized cutaneous disease, those with increased risk of systemic disease, and those who develop systemic disease [3]. Multi-agent systemic chemotherapy, compared to single agent, does not result in a higher cure rate nor prevent future relapses [2, 8].
Overall prognosis for primary cutaneous CD30-positive anaplastic large T-cell lymphoma is excellent. However, multifocal disease at presentation has a two-fold increased chance to acquire extracutaneous disease and a four-fold increased chance of mortality from the lymphoma [3, 8]. Anatomic site, size, cytology, and additional immunologic markers have not been shown to influence clinical behavior [3, 4]. Spontaneous regression and age less than 60 years are associated with a favorable prognosis [10]. Overall, primary cutaneous CD30+ large T-cell lymphoma survival at 5 and 10 years is 95 percent [8]. Because a risk for systemic progression exists, albeit low, longitudinal observation is strongly recommended.
Our patient had a relatively large CD30+ plaque. Clinical presentation with immunohistologic confirmation supported diagnosis as CD30+ large T-cell lymphoma. Although known to spontaneously regress, the recommendation for conservative radiation was implemented because of the low risk of systemic spread. This case has been presented for review of CD30+ large T-cell tumors.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
References
1. Fung MA, Murphy MJ, Hoss DM, Grant-Kels JM. Practical evaluation and management of cutaneous lymphoma. J Am Acad Dermatol 2002; 46: 325-57. PubMed2. Beljaards RC, Kaudewitz P, Berti E, Gianotti R, Neumann C, Rosso R, Paulli M, Meijer CJ, Willemze R. Primary cutaneous CD30-positive large cell lymphoma: definition of a new type of cutaneous lymphoma with a favorable prognosis. Cancer 1993; 71: 2097-104. PubMed
3. Willemze R, Beljaards RC. Spectrum of primary cutaneous CD30 (Ki-1)-positive lymphoproliferative disorders. J Am Acad Dermatol 1993; 28: 973-80. PubMed
4. Krishnan J, Tomaszewski MM, Kao GF. Primary cutaneous CD30-positive anaplastic large cell lymphoma. Report of 27 cases. J Cutan Pathol 1993; 20: 193-202. PubMed
5. Camisa C, Helm TN, Sexton C, Tuthill R. Ki-1-positive anaplastic large-cell lymphoma can mimic benign dermatoses. J Am Acad Dermatol 1993; 29: 696-700. PubMed
6. Strutton G. Cutaneous infiltrates-lymphomatous and leukemic. In: Weedon D, Strutton G, eds. Skin pathology. 2nd ed. Edinburgh: Churchill Livingstone: 2002: 1095-1138.
7. Willemze R, Meijer CJLM. Primary cutaneous CD30-positive lymphoproliferative disorders. Hematol Oncol Clin N Am 2003; 17: 1319-32. PubMed
8. Bekkenk MW, Geelen FA, Van Voorst Vader PC, Heule F, Geerts M, Van Vloten WA, Meiher CJLM, Willemze R. Primary and secondary cutaneous CD30-positive lymphoproliferative disorders: a report from the Dutch Cutaneous Lymphoma Group on the long-term follow-up data of 219 patients and guidelines for diagnosis and treatment. Blood 2000; 95: 3653-61. PubMed
9. Vonderheid EC, Sajjadian A, Kadin ME. Methotrexate is effective therapy for lymphomatoid papulosis and other primary cutaneous CD30-positive lymphoproliferative disorders. J Am Acad Dermatol 1996; 34: 470-81. PubMed
10. Paulli M, Berti E, Rosso R, Boveri E, et al. CD30/Ki-1-positive lymphoproliferative disorders of the skin - clinicopathologic correlation and statistical analysis of 86 cases: a multicentric study from the European Organization for Research and Treatment of Cancer Cutaneous Lymphoma Project Group. J Clin Oncol 1995; 13: 1343-54. PubMed
© 2006 Dermatology Online Journal