Necrobiotic xanthogranuloma of the chest wall
Published Web Location
https://doi.org/10.5070/D32rb3t35bMain Content
Necrobiotic xanthogranuloma of the chest wall
H Garth Smith DMD MD, Larry A Sargent MD, Daryl B Lundgrin MD
Dermatology Online Journal 12 (1): 12
The Department of Plastic and Reconstructive Surgery, The University of Tennessee College of Medicine - Chattanooga Unit.
UTPlastics@thepsg.orgAbstract
Necrobiotic xanthogranuloma is a rare disease that usually presents with indurated yellow red nodules or plaques in the dermis or subdermal tissues. The pathogenesis of this disease is unknown and the limited number of cases has made long-term studies difficult. We report the case of a 61-year-old woman seen in our office for a 5 × 5-cm lesion of her chest wall. Biopsies established a diagnosis of necrobiotic xanthogranuloma. The patient received 4 months of intralesional steriod injections without change in the lesion. The patient was also treated with colchicine for several months without improvement. Therefore, the lesion was surgically excised and the area was reconstructed with local advancement skin flaps. The patient has been followed for 2 years with no evidence of recurrence.
Introduction
Necrobiotic xanthogranuloma (NXG) is a disease characterized by indurated, violaceous yellow red nodules or plaques in the dermis or subdermal tissues. A rare disorder of histiocytic origin, NXG was first reported in 1980 [1]. The lesions are typically nontender and may show signs of central atrophy, ulceration, or telangiectasia. The lesions most commonly affected region is the periorbital area, but the lesions may involve the extremities and trunk [1, 2, 3, 4, 5]. NXG is a chronic disease that frequently progresses, having no preferred treatment options [2].
Clinical Synopsis
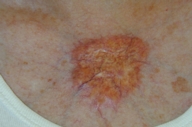
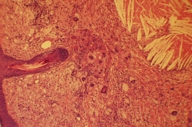
A 61-year-old woman presented with a 5 × 5-cm lesion of her anterior chest wall. A review of the patient's past medical and family history was unremarkable. The lesion had started as a painless, slightly discolored nodule on her anterior chest wall approximately 2 cm below the sternal notch. The lesion had slowly grown over the last 24 months to its current size on presentation. The patient underwent initial diagnostic studies by her dermatologist. Her laboratory tests were significant for slightly elevated liver function tests, slightly elevated IgG-κ and IgG-λ paraproteins, and elevated cholesterol levels (total and LDL). Prior punch biopsies of the lesion established a diagnosis of necrobiotic xanthogranuloma. Subsequent to this diagnosis the patient underwent 4 months of intralesional steroid injections without improvement. The patient was further treated with colchicine (0.6 mg b.i.d) for several months with no change in the lesion. Given her lack of response to treatment and her apprehension at using more potentially toxic chemotherapeutic agents, the patient was referred for surgical removal of the lesion. Physical examination revealed a 5 × 5-cm raised plaque containing yellowish nodules and areas of telangiectasia on her sternum (Fig. 1). Under general anesthesia the lesion was excised down to fascia with 1-cm peripheral margins. Histopathologic evaluation revealed a prominent granulomatous infiltrate diffusely involving the dermis and extending into the subcutaneous fat. The epithelium was noted to be atrophic (Fig. 2). Sheets of lipidized histiocytes intermixed with giant cells in a wreath-like configuration (Touton bodies) were identified (Fig. 3). Focal areas of necrobiosis and cholesterol clefting were also evident (Fig. 4). These features are consistent with a diagnosis of NXG. The resulting 6 × 6-cm defect was reconstructed utilizing local advancement skin flaps and healed without complications (Fig. 5). The patient has been followed for 2 years with no evidence of recurrence.
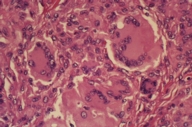 | 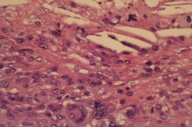 |
| Figure 3 | Figure 4 |
|---|---|
| Figure 3. Sheets of histiocytes intermixed with giant cells in a wreath like configuration (Touton bodies). | |
| Figure 4. Focal areas of necrobiosis and cholesterol clefting. | |
 |
| Figure 5 |
|---|
| Figure 5. Patient 24 months after local advancement flap reconstruction. |
Discussion
Necrobiotic Xanthogranuloma is a disease characterized by indurated, violaceous yellow red nodules or plaques in the dermis or subdermal tissues. A disorder of histiocytic origin, NXG was first reported in 1980 [1]. The lesions are typically nontender and may show signs of central atrophy, ulceration, or telangiectasia. NXG is a chronic disease that frequently progresses, having no preferred treatment options [2]. The pathogenesis of the disease is unknown [3, 6]. Many theories have been described to account for the development of the characteristic skin lesions, but none can account for all the patients thus far identified [3]. Patients who have gone on to develop granulomas of pulmonary or myocardial tissues, suggest a predilection for granuloma formation in NXG [4, 6]. The onset of symptoms occurs on average between 50 to 60 years of age, with the same incidence for men and women [5]. The lesions are most often located around the periorbital region (~80 %), but may involve the flexural extremities or trunk [1, 2, 3, 4, 5]. The clinical presentation may be accompanied by various hematologic disorders, including neutropenia, hypocomplimentemia, cryoglobulinemia, and hyperlipidemia [7]. The most often associated laboratory finding (> 70 %) is a monoclonal paraproteinemia, which tends to be either a κ- or λ-IgG monoclonal gammopathy [3, 4, 6]. There is a strong association between NXG and the development of certain malignancies. Long-term studies of NXG are limited given the rarity of the disorder. However, one study performed over a 17-year period followed 26 patients. Ten patients went on to develop a malignancy [7]. The most common associated systemic conditions include multiple myeloma, chronic lymphocytic leukemia, Hodgkin disease, non-Hodgkin lymphoma, asthma, and Quincke edema [7].
The treatment options for necrobiosis xanthogranuloma are diverse, although a single best treatment has yet to be identified. Treatment methods reported in the literature include the use of local corticosteroid injections, radiation therapy, plasmapheresis, surgical excision, chemotherapy with methotrexate, melphalan, chlorambucil [3, 5, 6], azathioprine, cyclophosphmide, nitrogen mustard, prednisone, and colchicines [7]. Responses to various treatment modalities have been mixed. Treatments appear to be palliative, with most patients exhibiting a slowly progressive course [7]. Our patient elected to undergo surgical excision of the lesion, although the rate of recurrence is reportedly high (~40 %) [7]. After 24 months of follow-up the patient has remained symptom free.
References
1. Kossard S., Winkelmann, R.K. Necrobiotic xanthogranuloma with paraproteinemia. J Am Acad Dermatol. 1980 Sep; 3(3):257-70. PubMed2. Venencie P.Y., Le Bras, P., Toan N.D., Tchernia G., Delfraissy J.F. Recombinant interferon alfa-2b treatment of necrobiotic xanthogranuloma with paraproteinemia. J Am Acad Dermatol. 1995 Apr; 32 (4): 666-7. PubMed
3. Russo, G.G. Necrobiotic Xanthogranuloma with Scleroderma. Cutis. 2002 Dec; 70 (6): 311-6. PubMed
4. Daoud M.S., Lust J.A., Kyle R.A., Pittelkow M.R. Monoclonal gammopathies and associated skin disorders. J Am Acad Dermatol. 1999 Apr; 40 (4): 507-535; quiz 536-8. PubMed
5. Mehregan D.A,, Winkelmann R.K. Necrobiotic Xanthogranuloma. Arch Dermatol. 1992 Jan; 128 (1): 94-100. PubMed
6. Burdick A.E., Sanchez J., Elgart G.W. Necrobiotic Xanthogranuloma Associated With A Benign Monoclonal Gammopathy. Cutis. 2003 Jul; 72 (1): 47-50. PubMed
7. Ugurlu S, BartleyG.B., Gibson L. Necrobiotic xanthogranuloma: long-term outcome of ocular and systemic involvement. Am J Ophthalmol. 2000 May; 129 (5): 651-7. PubMed
© 2006 Dermatology Online Journal