Naproxen-induced generalized bullous fixed drug eruption
Published Web Location
https://doi.org/10.5070/D32q83t60dMain Content
Naproxen-induced generalized bullous fixed drug eruption
Justin P Bandino MD, Wendi E Wohltmann MD, David W Bray MD, Aaron Z Hoover MD
Dermatology Online Journal 15 (11): 4
1. Transitional intern, San Antonio Military Medical Center (SAMMC), San Antonio, Texas. tantomed@gmail.com2. Dermatology resident, San Antonio Military Medical Center (SAMMC), San Antonio, Texas
3. Private practice dermatology, San Antonio, Texas
4. Chief of dermatopathology, San Antonio Military Medical Center (SAMMC), San Antonio, Texas
Abstract
A fixed drug eruption (FDE) is a cutaneous reaction to an ingested drug that recurs at the same site each time the offending drug is taken. Clinical diagnosis may be difficult as patients often do not consider over-the-counter medications or supplements as part of their reported medication list. In addition, patients may take the offending medication so infrequently that the eruption does not occur often enough to easily allow them to deduce the association. The most common offending agents include anti-microbials, non-steroidal anti-inflammatory drugs (NSAIDs), and anti-epileptics. Fixed drug eruptions classically present as a single, sharply demarcated, round erythematous patch or plaque, occasionally with localized bullae. Generalized bullous FDEs, however, are relatively rare and can be confused with Stevens-Johnson Syndrome. We present a case of naproxen-induced generalized bullous FDE in a 50-year-old woman.
Introduction
Naproxen sodium is a non-steroidal anti-inflammatory drug (NSAID) commonly used to alleviate pain, fever, or inflammation. NSAIDs are a commonly reported cause of fixed drug eruptions (FDEs), but the bullous and generalized variants are relatively rare. We present a case of a generalized bullous FDE due to naproxen.
Clinical synopsis
A 50-year-old woman presented with a 10-month history of an episodic, pruritic rash on her arms, chest, and feet. She recalled four previous eruptions, each lasting 2-3 weeks and then completely resolving without hyperpigmentation or scarring. She could not recall any associated triggers. However upon further questioning, she did note that the lesions occurred at the same sites each time. She had a past history of a nickel allergy, and current medications included cetirizine, lisinopril, hydrochlorothiazide, a multi-vitamin, fish oil, and occasionally naproxen for muscle aches.
Physical exam revealed multiple (>15), annular, 2-4 cm, erythematous patches on her bilateral upper extremities, back, chest, scalp, soft palate, and dorsal feet. Some patches had overlying tense bullae (Fig. 1B).
 |  |
| Figure 3 | Figure 4 |
|---|---|
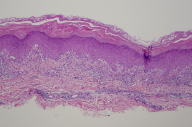
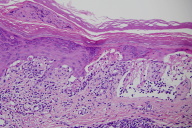
| Figure 3. Shave biopsy specimen from bullous lesion on right dorsal foot (H&E, x4) Figure 4. Shave biopsy specimen from bullous lesion on right dorsal foot (H&E, x20) | |
A shave biopsy was taken from a tense bulla on the patient's right dorsal foot and the specimen was sent for histologic evaluation.
Microscopic findings and clinical
Histopathologic examination of the specimen revealed an interface dermatitis along the dermal-epidermal junction with extensive subepidermal clefting and abundant necrotic keratinocytes.
Direct immunofluorescense revealed numerous cytoid bodies along the epidermal basement membrane zone that stained with IgM. Deposition of IgG, C3, IgA, C5b-9, or fibrinogen was not observed. At her follow-up visit, the patient remembered that the lesions recurred in the same locations each time and that she had taken the naproxen prior to each eruption. The patient was treated with fluocinonide 0.05 percent ointment BID, cetirizine every morning, and hydroxyzine at night. All lesions completely resolved within ten days. The patient was advised to discontinue naproxen.
Discussion
Fixed drug eruption is a cutaneous reaction to an ingested drug that recurs at the same site each time the offending drug is taken. Clinical diagnosis may be difficult because patients often do not consider over-the-counter medicines or supplements as part of their medication regimen when reporting their medical history. Patients also may take a medication so infrequently, as in the case of our patient, that the eruption does not occur often enough to easily suggest the association. Fixed drug eruptions typically present as a single, sharply demarcated, round, erythematous patch or edematous plaque with a dusky red hue. Burning or pruritis may accompany the lesions, but systemic symptoms are typically not present. Violaceous to brown post-inflammatory hyperpigmentation usually follows healing, although nonpigmenting lesions have been reported, mostly from pseudoephedrine [1]. Our patient did not have clinically ostensible post-inflammatory hyperpigmentation, but histological pigmentary incontinence was present.
Histologically, FDE is an interface dermatitis with prominent vacuolar change along the dermal-epidermal junction with keratinocyte necrosis and pigment incontinence. The bullous variant results when extensive subepidermal clefting is present. Because of the acute onset, the stratum corneum typically demonstrates orthokeratosis, although in established lesions parakeratosis can be present. The inflammatory infiltrate is predominately lymphocytic but often includes eosinophils and neutrophils. The infiltrate typically extends into the mid-reticular dermis, and biopsies of lesions after re-exposure demonstrate dermal fibrosis and pigment around vessels. Similar histological findings can been seen in erythema multiforme, but findings that favor FDE are the mixed nature of the infiltrate, deeper extension into the dermis, dermal fibrosis, and the presence of pigment incontinence around vessels [2].
Numerous drugs have been implicated to cause FDEs; these include antibacterials, antifungals, antiepileptics, anti-inflammatory drugs, and herbal supplements [3]. An FDE has even been reported following an influenza vaccination [4]. In recent studies, the most common offending agents were antimicrobials (39-65%) such as co-trimoxazole and dapsone, NSAIDs (16-35%), and antiepileptics (16-30%) [5, 6, 7].
If the diagnosis is uncertain, FDEs can be recreated with small increasing systemic doses of the offending agent, but a generalized eruption may result. Patch testing or intradermal skin testing are alternative methods to confirm the diagnosis [8]. Time of onset of a patient's FDE can take days to weeks after first exposure to the offending drug, although FDEs typically present within minutes to hours (mean 2.1 hours) after subsequent exposures [9]. Any skin or mucous membrane site can be involved, but some drugs are known to induce FDEs at specific sites. Tetracycline, for example, typically induces a solitary lesion on the glans penis [10]. In approximately 30 percent of cases, an FDE will present with localized bullae [11]. A generalized bullous FDE, however, is relatively rare, and when this occurs it can be confused with Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis [12, 13]. Naproxen-induced generalized bullous FDE is an uncommonly reported reaction [14, 15].
The pathogenesis of FDEs is not well understood. However, one recent article cites two cases of FDE and one of bullous FDE that occurred in locations of prior cutaneous trauma. The authors theorized that the fixed areas may be sites of lowered cutaneous resistance to the offending drug, potentially induced by prior infectious, vascular, immunological, or neural insults to the area [16]. Genetic predisposition may also play a causative role and is suggested by reports of similar lesions among family members and HLA type associations [17, 18].
Conclusion
Fixed drug eruptions are cutaneous reactions that can be difficult to diagnose because of the wide variety of possible offending drugs, a varied time course of onset after exposure, and the potential for infrequent use of the causative drug. Obtaining a thorough history and a full medication list to include supplements and OTC drugs are thus highly effective tools to indicate the correct diagnosis.
References
1. Shelley WB, Shelley ED. Nonpigmenting fixed drug eruption as a distinctive reaction pattern: examples caused by sensitivity to pseudoephedrine hydrochloride and tetrahydrozoline. J Am Acad Dermatol. 1987 Sep;17(3):403-7. [PubMed]2. Korkij W, Soltani K. Fixed drug eruption: A brief review. Arch Dermatol. 1984 Apr;120(4):520-4. [PubMed]
3. Sehgal VN, Srivastava G. Fixed drug eruption (FDE): changing scenario of incriminating drugs. Int J Dermatol. 2006 Aug;45(8):897-908. [PubMed]
4. Garcia Doval I, Roson E, Feal C, De la Torre C, Rodriguez T, Cruces MJ. Generalized bullous fixed drug eruption after influenza vaccination, simulating bullous pemphigoid. Acta Derm Venereol. 2001 Nov-Dec;81(6):450-1. [PubMed]
5. Gupta R. Drugs causing fixed drug eruptions: confirmed by provocation tests. Indian J Dermatol Venereol Leprol. 2003 Mar-Apr;69(2):120-121. [PubMed]
6. Pudukadan D, Thappa DM. Adverse cutaneous drug reactions: clinical pattern and causative agents in a tertiary care center in South India. Indian J Dermatol Venereol Leprol. 2004 Jan-Feb;70(1):20-24. [PubMed]
7. Patel RM, Marfatia YS. Clinical study of cutaneous drug eruptions in 200 patients. Indian J Dermatol Venereol Leprol. 2008 Jul-Aug;74(4):430. [PubMed]
8. Osawa J, Naito S, Aihara M, Kitamura K, Ikezawa Z, Nakajima H. Evaluation of skin test reactions in patients with non-immediate type drug eruptions. J Dermatol. 1990 Apr;17(4):235-9. [PubMed]
9. Stubb S. Blood leukocytes, with special reference to basophils and eosinophils, during provocation tests in fixed eruption and drug exanthema. Acta Derm Venereol Suppl (Stockh). 1976;56(76):1-47. [PubMed]
10. Thankappan TP, Zachariah J. Drug-specific clinical pattern in fixed drug eruptions. Int J Dermatol. 1991 Dec;30(12):867-70. [PubMed]
11. Kauppinen K. Cutaneous reactions to drugs with special reference to severe bullous mucocutaneous eruptions and sulphonamides. Acta Derm Venereol (Stockh). 1972;68:1-89. [PubMed]
12. Lisi P, Stingeni L. Fixed Drug Eruption: Bullous Form. Clinics in Dermatol. 1993 Oct-Dec;11(4):461-6. [PubMed]
13. Rai R, Jain R, Kaur I, Kumar B. Multifocal bullous fixed drug eruption mimicking Stevens-Johnson syndrome. Indian J Dermatol Venereol Leprol. 2002 May-Jun;68(3):175-6. [PubMed]
14. Leivo T, Heikkila H. Naproxen-induced generalized bullous fixed drug eruption. Br J Dermatol. 2004 Jul;151(1):232. [PubMed]
15. Gonzalo Garijo MA, Bobadilla Gonzalez P. Cutaneous reaction to naproxen. Allergol Immunopathol (Madr). 1996 Mar-Apr;24(2):89-92. [PubMed]
16. Kim SY, Kang H, Kim HO, Park YM. Bullous fixed drug eruption localized to the skin graft sites. J Eur Acad Dermatol Venereol. 2008 Dec;22(12):1503-4. Epub 2008 Mar 18. [PubMed]
17. Pellicano R, Silvestris A, Iannantuono M, Ciavarella G, Lomuto M. Familial occurrence of fixed drug eruptions. Acta Derm Venereol. 1992 Aug;72(4):292-3. [PubMed]
18. Pellicano R, Ciavarella G, Lomuto M, Di Giorgio G. Genetic susceptibility to fixed drug eruption: evidence for a link with HLA-B22. J Am Acad Dermatol. 1994 Jan;30(1):52-4. [PubMed]
© 2009 Dermatology Online Journal



