Eccrine porocarcinoma
Published Web Location
https://doi.org/10.5070/D32j0313pmMain Content
Eccrine porocarcinoma
AG Affleck1, J L Bong1, M A Ostroumova2, IH Leach3, A G Perks4, S Varma1
Dermatology Online Journal 12 (1): 17
1. Department of Dermatology, Queen's Medical Centre, Nottingham, UK. marsha@doctors.org.uk 2. Bristol Dermatology Centre,
Bristol, UK 3. Department of Histopathology, Queen's Medical Centre, Nottingham, UK 4. Department of Plastic Surgery, Nottingham
City Hospital. Nottingham, UKAbstract
We present an unusual case of eccrine porocarcinoma in that diagnosis was delayed for many years after the initial lesion appeared, resulting in relatively large tumor.
Introduction
A 68-year old man presented with an 8-year history of an enlarging lesion on his right leg. Recent onset of malodor and discharge prompted his consultation. Physical examination revealed a large, red, exophytic, circumscribed tumor.
 |
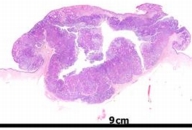
| Figure 1 |
|---|
| A large, pink, exophytic, circumscribed tumor |
An excision biopsy was performed (Fig. 2). Histology showed a polypoid tumor composed of small uniform cells involving epidermis and dermis. Focal ductal differentiation was present and the appearances were typical for eccrine poroma. In addition, there was a focal nuclear atypia and invasion in to dermis and subcutis (Fig. 3). There was no vascular or perineural invasion and the lesion was completely excised. The patient is being followed and there has been no evidence of recurrence to date (12 months).
 | 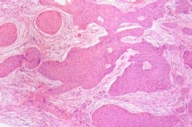 |
| Figure 2 | Figure 3 |
|---|---|
| Figure 2. A large exophytic tumor showing invasion into subcutis to a depth of 29 mm Figure 3. An invasive malignant epithelial tumor showing extensive ductal differentiation. | |
Discussion
Skin adnexal tumors are uncommon and seldom are allowed to become so large. Their clinical appearance is usually nonspecific and the majority are diagnosed histologically. Eccrine poroma and porocarcinoma, however, often have a pink, moist, shiny surface that is a diagnostic clue.
Eccrine porocarcinoma, previously known as malignant eccrine poroma or eccrine adenocarcinoma, is a rare malignant tumor arising from the intraepidermal portion of the eccrine sweat gland duct epithelium [1, 2]. The tumor most often occurs in the elderly with average age at diagnosis between 60 and 80 years [3].
Some porocarcinomas arise from a pre-existing benign lesion (eccrine poroma) manifesting with recent increase in size, tenderness, and (rarely) becoming malodorous [1]. The average time from tumor onset to treatment varies, reported in a recent series to be 4 years [3].
The clinical appearance of this rare neoplasm varies—it can appear as a nodule, a dome-shaped, infiltrated or erosive plaque, or as a polypoid growth that tends to ulcerate. The average size of primary tumor is 2.4 cm [4]. Clinical differential diagnoses include cutaneous squamous cell carcinoma, cutaneous lymphoma, extramammary Paget's disease, Bowen's disease, cutaneous metastases, amelanotic melanoma, or other primary skin-appendage tumor.
It was previously thought that the majority of porocarcinomas are found on the palms and soles, reflecting the high concentration of sweat glands. However, the distribution of these lesion appears to have no correlation with sweat gland density; around 50 percent occur on lower extremities, a further 20 percent on head and neck and upper limbs and 12 percent on the trunk and the abdomen [2, 3]. Eccrine differentiation of many sweat gland tumors is controversial. They may arise from follicullo-sebaceous-apocrine germ and therefore show apocrine rather than eccrine differentiation. Indeed, it is suggested that the adjective eccrine is not used and that the name of this tumor is simply porocarcinoma [5].
Eccrine porocarcinoma has metastatic potential and a propensity for local recurrence, and is noted to have invasion of dermal lymphatic vessels early in the disease process [5]. There is also a propensity for epidermotropic metastases. However, a large case series of eccrine porocarcinoma suggests that the incidence of an aggressive clinical course is less than previously believed, with a regional metastatic rate of only 20 percent. Once metastasized, however, prognosis is poor with a mortality rate of 75-80 percent according to a large case series [5, 6].
Eccrine porocarcinoma, although a rare neoplasm, should always be considered in the differential diagnosis of any moist exophytic tumor, especially in the elderly. In all suspected cases the treatment of choice is excision.
Eccrine porocarcinoma learning points typically has a pink, moist, shiny surfacemay present as a chronic enlarging tumor
may develop an exophytic appearance
References
1. Shaw M, McKee PH, Lowe D, et al. Malignant eccrine poroma - a study of 27 cases. Br J Dermatol 1982; 107: 675-80.2. Mehregan AH, Hasimoto K, Homayoon R. Eccrine adenocarcinoma- a clinicopathologic study of 35 cases. Arch Dermatol 1983; 119: 104-114.
3. Perna C, Cuevas J, Jimenez-Heffernan JA et al. Eccrine porocarcinoma (malignant eccrine poroma). Am J Surg Path 2002; 26: 272-4.
4. Huet P, Dandurand M, Pignodel C et al. Metastasizing eccrine porocarcinoma. J Am Acad Dermatol 1996; 35: 860-864.
5. Harvell JD, Keroehmann RL, LeBoit PE. Eccrine or apocrine poroma? Six poromas with divergent adnexal differentiation. Am J Dermatopath. 1996; 18: 1-9.
6. Robson A, Greene J, Ansari N et al. Eccrine porocarcinoma (malignant eccrine poroma): a clinicopathologic study of 69 cases. Am J Surg Pathol 2001; 25: 710-20.
© 2006 Dermatology Online Journal

