Primary cutaneous marginal zone b-cell lymphoma: An atypical case
Published Web Location
https://doi.org/10.5070/D32h711434Main Content
Primary cutaneous marginal zone b-cell lymphoma: An atypical case
Diana Velázquez1, Pilar de Pablo2, Diana García2, José Ramón Ramírez3
Dermatology Online Journal 16 (12): 5
1. Department of Dermatology, Infanta Leonor Hospital, Madrid, Spain. diana_velazquezt@yahoo.es2. Department of Dermatology, Tajo Hospital, Madrid, Spain
3. Department of Pathology, Tajo Hospital, Madrid, Spain
Abstract
Primary cutaneous marginal zone B-cell lymphoma (PCMZBCL) is an entity with an indolent behavior, which clinically appears as erythematous papules, nodules, or plaques, solitary or multiple, on the trunk or upper extremities. It has been associated with autoimmune diseases and infections. We present the case of a 77-year-old woman with an atypical PCMZBCL with extracutaneous spread and associated autoimmune hemolytic anemia.
Case report
A 77-year-old woman with a ten-year history of autoimmune hemolytic anemia being treated with rituximab, visited our department complaining of asymptomatic skin lesions, which had progressively enlarged over the last 10 years. The plaques affected the left side of the thorax, axilla, and shoulder blade. These lesions started at the same time the autoimmune hemolytic anemia was diagnosed.
Physical examination revealed 3 erythematous, telangiectatic, infiltrated and diffuse plaques, affecting the left side of the thorax, axilla, and scapula (Figures 1 and 2).
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figures 1 and 2. Erythematous, telangiectatic, infiltrated, and diffuse plaques, affecting the left side of the thorax and scapula | |
Laboratory analysis showed: WBC: 4.700/mm³, Hb: 13.6g/dl, LDH and SGOT slightly high, and β2-microglobulin within normal range all likely related to the autoimmune hemolytic anemia.
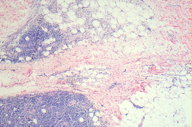
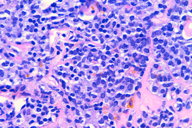
Histological examination showed a lymphoid neoplasm involving deep dermis and subcutis, composed of small to intermediate size lymphocytes with centrocyte-like features, lymphoplasmacytoid lymphocytes, and plasma cells (Figures 3 and 4). By immunohistochemistry, almost all of the cells showed reactivity for CD20, CD79 alpha, and BCL-2. Expression of cycline D1, CD10, and BCL-6 was negative.
Systemic examination included a CT scan and a bone marrow biopsy, which showed no alteration. There was neither hepatomegaly nor splenomegaly, but a mammography revealed an irregular high-density nodule in left axilla, not seen in a previous mammography in 2004. The ultra sound scan and the bilateral breast magnetic resonance imaging confirmed a 9 mm irregular subcutaneous nodule in the distal left breast, with a similar lymphoid infiltration to the one observed in the skin.
According to these findings, the patient was diagnosed with primary cutaneous marginal zone B-cell lymphoma (PCMZL). Consultant hematologists initiated therapy with chlorambucil 6 mg daily for four months. A partial response was observed and the patient remains stable after a 10-month follow up.
Discussion
The primary cutaneous marginal zone B-cell lymphoma (PCMZL) is a low grade malignant lymphoma of the skin; there is generally no evidence of extracutaneous disease at least 6 months after diagnosis [1]. The condition is characterized by a clonal proliferation of small B lymphocytes, including marginal zone cells (centrocyte-like), lymphoplasmacytoid cells, and plasma cells [2]. It is classified within the group of lymphomas of mucosal associated lymphoid tissue (MALT). These are low-grade B-cell lymphomas arising at extranodal sites, the most common being the gastrointestinal tract, lung, thyroid gland, conjunctiva, orbit, salivary gland, and skin [3].
Clinically, it appears more frequently as multifocal skin lesions instead of solitary lesions, showing predilection for the trunk and upper extremities. The tumors appear as red-brown papules, plaques, and nodules, although the early lesions can manifest as a nonspecific erythematous eruption [3].
Chronic antigenic stimulation is thought to be associated with the transformation and progression of this type of lymphoma [4]. In the case of cutaneous MALT lymphoma, it is believed that Borrelia burgdorferi plays some kind of role, because studies from European areas with endemic Lyme disease have demonstrated a greater prevalence of the spirochete in patients with PCMZL. Even nearly complete clinical and histologic regression of PCMZL has been observed after penicillin treatment against B. burgdorferi [5]; frequently PCMZL is associated with erythema chronicum migrans or acrodermatitis chronica atrophicans [2]. In contrast, this kind of association was not found in American and Asian cases. Apart from PCMZL, Borrelia ADN has also been found in cases of primary cutaneous follicular center cell lymphoma and diffuse large B-cell lymphoma [7].
As with infections, autoimmune conditions can also be considered to be associated factors in PCMZL development. In patients with Sjogren syndrome, characterized by a chronic inflammation of salivary or lachrymal glands, higher incidences of lymphomas have been observed at these sites [8]. Similarly, there has been detected a relationship between thyroid and lung lymphomas in patients with Hashimoto thyroiditis [9] and lymphoid interstitial pneumopathy [10]. Occasionally, PCMZL has been described in association with rheumatoid arthritis [11], chronic lymphocytic leukemia [12], and as an infiltration of the frontal bone [13].
The prognosis is excellent, with a 5-year survival rate of approximately 97 percent. However, skin relapses are frequent, about 48 percent [2] and much more common in patients who presented with multifocal skin lesions. Although extracutaneous spread is exceptional, there have been reported cases, even deaths, cause by disseminated disease. The extracutaneous involvement sites include other MALT areas such as the gastrointestinal system, lymph nodes, tonsils, spleen, orbits, salivary glands, bone marrow, or parotids [14].
The optimal treatment of PCMZL is unclear. The treatment choice usually depends on the involvement site, the age, and the general health of the patient. Lesions can be treated by radiotherapy, surgical excision, chlorambucil or polychemotherapy, interferon alpha or rituximab. A wait-and-see strategy is often followed, particularly in patients with frequent relapsing skin lesions, in the same way as with other indolent B-cell lymphomas and leukemias [2].
There are several particularities in this case. Firstly, clinically our patient exhibited erythematous, telangiectatic, infiltrated, and diffuse plaques instead of the typical erythematous nodules. This can be possibly justified with the more than 10-year lesion evolution.
Second, we must emphasize the extracutaneous spread to the left breast, which is very rare in these kinds of lymphomas. Although the patient already had the breast lesion at the time of the diagnosis, we consider the lymphoma as primary cutaneous because there was a normal mammography done the previous year.
Third, the patient describes the beginning of the cutaneous lesions at the same time the autoimmune hemolytic anemia was diagnosed. This association has not been described previously.
Finally, we would like to emphasize that the treatment used for the autoimmune hemolytic anemia was rituximab, which is also effective against PCMZL, but did not produce a positive result in this case.
References
1. Demierre MF, Kerl H, Willemze R. Primary cutaneous B-cell lymphomas: a practical approach. Hematol Oncol Clin North Am 2003; 17: 133-50. [PubMed]2. Hoefnagel JJ, Vermeer MH, Jansen PM et al. Primary cutaneous marginal zone B-cell lymphoma. Clinical and therapeutic features in 50 cases. Arch Dermatol 2005; 141: 1139-45. [PubMed]
3. Cho-Vega JH, Vega F, Rassidakis G et al. Primary cutaneous marginal zone B-cell lymphoma. Am J Clin Pathol 2006; 125: S38-S49. [PubMed]
4. Thieblemont C, Coiffier B. Management of marginal zone lymphomas. Curr Treat Options Oncol 2006; 7: 213. [PubMed]
5. Slater DN. Borrelia burgdorferi-associated primary cutaneous B-cell lymphoma. Histopathology 2001; 38: 73-7. [PubMed]
6. Picken RN, Strle F, Ruzic-Sabljic E et al. Molecular subtyping of Borrelia burgdorferi sensu lato isolates from five patients with solitary lymphocytoma. J Invest Dermatol 1997; 108: 92-7. [PubMed]
7. Goodlad JR, Davidson MM, Hollowood K et al. Primary cutaneous B-cell lymphoma and Borrelia burgdorferi infection in patients from Highlands of Scotlands. Am J Surg Pathol 2000; 24: 1279-85. [PubMed]
8. Theander E, Henriksson G, Ljungberg O et al. Lymphoma and other malignancies in primary Sjögren’s syndrome: a cohort study on cancer incidence and lymphoma predictors. Ann Rheum Dis 2006; 65: 796. [PubMed]
9. Hyjek E, Isaacson PG. Primary B-cell lymphoma of the thyroid and its relationship to Hashimoto’s thyroiditis. Hum Pathol 1988; 19: 1315. [PubMed]
10. Addis BJ, Hyjek E, Isaacson PG. Primary pulmonary lymphoma: a re-appraisal of its histogenesis and its relationship to pseudolymphoma and lymphoid interstitial pneumonia. Histopathology 1988; 13: 1. [PubMed]
11. Yildirim FE, Karadumam A, Hürmüz P et al. Symmetrical primary cutaneous marginal zone lymphoma associated with rheumatoid arthritis. J Cutan Pathol 2009; 5: 1-5. [PubMed]
12. Robak E, Jesionek-Kupnicka D, Robak T et al. Primary cutaneous marginal zone B-cell lymphoma in a patient with chronic lymphocytic leukaemia. Br J Dermatol 2007; 157: 591-5. [PubMed]
13. Hashimoto C, Nagai Y, Ando M et al. Primary cutaneous marginal zone B-cell lymphoma infiltrating the frontal bone. Eur J Dermatol 2007; 17; 100-1. [PubMed]
14. Demirkesen C, Tüzüner N, Su Ö et al. Primary cutaneous immunocitoma/marginal zone B-cell lymphoma: a case with unusual course. Am J Dermatopathol 2004; 26: 119-22. [PubMed]
© 2010 Dermatology Online Journal