Shiitake mushroom-induced flagellate erythema: A striking case and review of the literature
Main Content
Shiitake mushroom-induced flagellate erythema: A striking case and review of the literature
Audrey S Wang1 MD, Keira L Barr1,2 MD, Jared Jagdeo1,3,4 MD
Dermatology Online Journal 19 (4): 5
1. Department of Dermatology, University of California Davis, Sacramento, California2. Department of Pathology, University of California Davis, Sacramento, California
3. Dermatology Service, Sacramento Veterans Affairs Medical Center, Mather, California
4. Department of Dermatology, SUNY Downstate, Brooklyn, New York
Abstract
Ingestion of raw or undercooked shiitake mushrooms is associated with a distinctive flagellate erythema. We describe a 61-year-old Caucasian man who presented with a pruritic, erythematous eruption of multiple linear streaks on the trunk and extremities starting 1 day after eating raw shiitake mushrooms. His symptoms and skin lesions resolved with minimal hyperpigmentation within approximately 1 week after treating with topical steroids and oral antihistamines. Skin biopsy showed non-specific findings, including a sparse perivascular and interstitial dermatitis as well as focal vacuolar interface changes. Our case illustrates that this condition is a visibly striking dermatitis with a self-limited course. The pathomechanism of the skin eruption remains unclear.
Case report
Physical examination revealed a well-appearing, well-nourished, fair-skinned man with mild diffuse facial erythema as well as multiple erythematous, blanchable, macular, linear streaks most prominently on the abdomen and flanks. Areas of sparing were notable on the central back, chest, and axillae. Confluent blanchable erythematous patches covered the upper extremities and lower extremities, the latter to a lesser extent (Figures 1A, C, E). Scattered petechiae were noted on the flexural surfaces of the upper extremities.
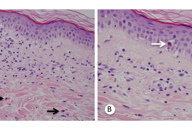
A punch biopsy obtained from an involved area on the left abdomen showed a sparse perivascular and interstitial dermatitis with eosinophils (Figure 2A, black arrows) and focal necrotic keratinocytes (Figure 2B, white arrow), consistent with vacuolar interface changes.
The patient’s pruritus improved on a regimen of triamcinolone 0.1 percent ointment applied twice daily and oral antihistamines. His skin eruption resolved with minimal hyperpigmentation within 1 week of his initial evaluation (Figures 1B, 1D, and 1F). The patient was advised to avoid eating raw shiitake mushrooms in the future to prevent recurrence.
Discussion
First reported by Nakamura in 1977 [1], ingestion of raw or undercooked shiitake mushrooms can induce flagellate erythema, also known as shiitake dermatitis. The eruption often occurs within the first 2 days after ingestion of the mushroom and is frequently pruritic. However, there is no mucosal involvement. Areas of sparing on the back suggest trauma-related skin changes from scratching [2].
The exact pathomechanism of this condition is unclear. Previous reports proposed a toxin-mediated phenomenon or increased interleukin-1 secretion induced by the polysaccharide lentinan in shiitake mushrooms, causing vasodilation and hemorrhage [3]. Patch testing and skin prick testing have not proven useful for diagnosing this condition [2], suggesting a non-allergic etiology. As in our case, non-specific histopathologic features have been described, including papillary dermal edema [4]; dermal perivascular cell infiltrate of lymphocytes, neutrophils, eosinophils, and histiocytes; spongiosis; and elongation of the rete ridges [5]. Thus, the diagnosis is usually made based on clinical history and physical examination.
Shiitake mushroom-induced flagellate erythema is thought to spontaneously resolve within 1 to 3 weeks [4, 6]. Our patient improved with symptomatic management using topical steroids and oral antihistamines, but others have reported using short-term balneo psoralen ultraviolet A (PUVA) phototherapy with rapid alleviation of pruritus [6].
Notably, the chemotherapeutic agent bleomycin can also cause flagellate hyperpigmentation, lasting several months [7]. In contrast, shiitake dermatitis typically does not cause hyperpigmentation [5].
Conclusion
Shiitake mushroom-induced flagellate erythema is an intriguing condition with a distinctive cutaneous manifestation but poorly understood pathogenesis. Overall, this condition appears to be benign based on its self-limited course and absence of long-term sequelae. Our case illustrates the rapidity with which shiitake mushroom-induced flagellate erythema can resolve with symptomatic treatment and discontinuation of the trigger.
References
1. Nakamura, T., Toxicoderma caused by shiitake (Lentinus edodes). Jpn J Clin Dermatol., 1977. 31(2): p. 65-68.2. Nakamura, T., Shiitake (Lentinus edodes) dermatitis. Contact Dermatitis, 1992. 27(2): p. 65-70. [PubMed]
3. Hanada, K. and I. Hashimoto, Flagellate mushroom (Shiitake) dermatitis and photosensitivity. Dermatology, 1998. 197(3): p. 255-7. [PubMed]
4. Lippert, U., et al., Shiitake dermatitis. Br J Dermatol, 2003. 148(1): p. 178-9. [PubMed]
5. Girard, C. and D. Bessis, Flagellate dermatitis. Shiitake dermatitis (toxicoderma). Arch Dermatol, 2010. 146(11): p. 1301-6. [PubMed]
6. Scheiba, N., M. Andrulis, and P. Helmbold, Treatment of shiitake dermatitis by balneo PUVA therapy. J Am Acad Dermatol, 2011. 65(2): p. 453-5. [PubMed]
7. Polla, B.S., et al., Flagellate pigmentation from bleomycin. J Am Acad Dermatol, 1986. 14(4): p. 690. [PubMed]
© 2013 Dermatology Online Journal