Pigmented Lesion in the inguinal region
Published Web Location
https://doi.org/10.5070/D323q2r503Main Content
Pigmented Lesion in the inguinal region
Nadia El Fekih MD, Abdelmooti Hawiloo MD, Soumeya MD Remmah, Rachida Zermani MD, Becima Fazaa MD
Dermatology Online Journal 17 (11): 12
Charles Nicolle Hospital Tunis, Tunis, TunisiaAbstract
Pigmented Bowen disease (PBD) is a rare tumor characterized by increased melanin pigment in the epidermis or papillary dermis in addition to the typical findings of Bowen disease. We report the case of a 60-year-old woman who presented with a 6-month history of a gradually enlarging solitary dark brown plaque in her right inguinal region. Histopathology showed hyperkeratosis with parakeratosis, acanthosis, disorganization of epidermal architecture, atypical keratinocytes, and increased melanin pigment of the papillary dermis. Considering the clinical and the histological evidence, a diagnosis of PBD was established. Complete resection confirmed the diagnosis. Pigmented Bowen disease is an unusual form of squamous carcinoma in situ. Other tumors in the differential diagnosis include pigmented basal cell carcinoma and superficial spreading melanoma.
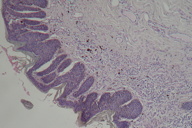
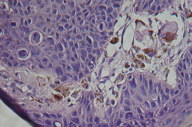
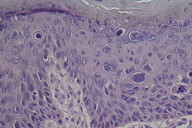
A previously healthy 60-year-old woman presented to our dermatology department with a 6-month history of a gradually enlarging solitary dark brown plaque in her right inguinal region. There was no history of neoplasm or nor chronic arsenical exposure. Clinical examination showed an asymmetric, brown plaque, 1 x 2 cm in size, with irregular borders, verrucous surface, and varied pigmentation (Figure 1). The lesion was painless. Physical examination showed no peripheral adenopathy or signs of metastasis. Chest radiography, abdominal, and inguinal echography, as well as laboratory blood tests (Hemogram, blood glucose, renal, and liver parameters), were normal. The histopathologic findings showed hyperkeratosis with parakeratosis, acanthosis, disorganization of epidermal architecture, atypical keratinocytes (Figure 2), and increased melanin pigment of the papillary dermis (Figures 3 and 4).
 |  |
| Figure 3 | Figure 4 |
|---|---|
| Figure 3. Melanin pigment of the papillary dermis (Optical microscopy, x10) Figure 4. Melanin pigment of the papillary dermis (Optical microscopy, x40) | |
Case report
On the basis of the clinical appearance, the differential diagnosis included pigmented basal cell carcinoma or superficial spreading melanoma. She was referred to the department of Plastic Surgery and a complete excision with 5 mm margin was performed.
Considering the clinical and histological picture, a diagnosis of Pigmented Bowen disease (PBD) was confirmed. There has been no evidence of recurrence at the 3-month follow-up.
Pigmented Bowen disease (squamous cell carcinoma in situ) is an uncommon tumor characterized by increased melanin pigment in the epidermis or papillary dermis in addition to the typical findings of Bowen disease [1]. Ragi et al found the pigmented variant to represent 1.67 percent of their 420 collected cases of cutaneous Bowen disease [2]. As in our patient, this type of lesion presents as a hyperpigmented, sharply marginated plaque with a surface that may be velvety, verrucous, or flat; it is generally asymptomatic [3]. When a non sun-exposed area such as the inguinal region is affected, chronic arsenic exposure, immunosuppression, and HPV infection should be considered [3]. Also, our patient had no history of chronic arsenic intoxication, trauma, or exposure to radiation, but immunohistochemical staining for HPV was not made.
The etiology of the pigment in BD is unclear. It has been suggested that the neoplastic cells may produce specific factors or cytokines that induce the proliferation of melanocytes and stimulate melanin production [4]. In our case, melanocytic proliferation was not observed.
Pigmented Bowen disease should be differentiated from other pigmented lesions like pigmented actinic keratosis, seborrheic keratoses, different types of melanocytic nevi, basal cell carcinomas, and melanoma [5, 6]. Histology remains the gold standard for an accurate diagnosis. Generally, PBD shows epidermal dysplasia with abnormal keratinization [7, 8]. The dermis shows no invasion of tumor cells. There are characteristically abundant melanin-rich cells in the basal layer. Significant quantities of melanin may be found within the epidermal cells of the basal layer, within the dermal melanophages or within the melanocytes in the affected epithelium [4, 7]. In our case, histologic examination revealed increased in dermal melanophages.
In 2004, Zalaudek et al described the dermoscopic findings of PBD [5]. Cameron et al, after studying 53 patients with PBD, concluded that a linear arrangement of brown and/or gray dots and/or coiled vessels was a specific clue of PBD, in particular allowing differential diagnosis from melanoma [9]. Nevertheless, differentiating between PBD and other pigmented lesions by dermoscopy may be difficult [10].
Various treatment modalities are widely in use for the treatment of this disease, but the surgical modalities seem to provide the best treatment with the highest cure rate. Cautery, cryotherapy, topical agents like 5-FU, and imiquimod have been reported to be effective in individual cases, but there are no controlled clinical studies demonstrating the efficacy of these treatments [11]. Standard excision was performed for our patient and there has been no evidence of recurrence at the 3-month follow-up.
In conclusion, PBD, even if unusual, should be considered in the differential diagnosis of pigmented skin lesions.
References
1. Lee JW, Hur J, Yeo KY, Yu HJ, Kim JS. A Case of Pigmented Bowen's Disease. Ann Dermatol. 2009 ;21:197-9 [PubMed]2. Ragi G, Turner MS, Klein LE, Stoll HL Jr. Pigmented Bowen's disease and review of 420 Bowen's disease lesions. J Dermatol Surg Oncol 1988;14:765-769. [PubMed]
3. Stante M, de Giorgi V, Massi D, Chiarugi A, Carli P. Pigmented Bowen's disease mimicking cutaneous melanoma: clinical and dermoscopic aspects. Dermatol Surg 2004;30: 541-544. [PubMed]
4. Firooz A, Farsi N, Rashighi-Firoozabadi M, Gorouhi F. Pigmented Bowen's disease of the finger mimicking malignant melanoma. Arch Iran Med 2007; 10:255-257. [PubMed]
5. Zalaudek I, Argenziano G, Leinweber B, Citarella L, Hofmann-Wellenhof R, Malvehy J, et al. Dermoscopy of Bowen's disease. Br J Dermatol 2004;150:1112-6. [PubMed]
6. Chapman MS, Quitadamo MJ, Perry AE. Pigmented squamous cell carcinoma. J Cutan Pathol. 2000;27:93-5. [PubMed]
7. Papageorgiou PP, Koumarianou AA, Chu AC. Pigmented Bowen's disease. Br J Dermatol 1998;138:515-518. [PubMed]
8. Pai VV, Hanumanthayya K, Naveen KN, Rao R, Dinesh US. Bowen's disease over the abdomen - A histological pigmented variety. Indian J Cancer 2011;48:121-2 [PubMed]
9. Cameron A, Rosendahl C, Tschandl P, Riedl E, Kittler H. Dermatoscopy of pigmented Bowen's disease. J Am Acad Dermatol. 2010;62: 597-604. [PubMed]
10. Hu SC, Chiu HH, Chen GS, Ke CL, Cheng ST. Dermoscopy as a diagnostic and follow-up tool for pigmented Bowen's disease on acral region. Dermatol Surg 2008; 34:1248-53. [PubMed]
11. Moreno G, Chia AL, Lim A, Shumack S. Therapeutic options for Bowen's disease. Australas J Dermatol 2007;48:1-10. [PubMed]
© 2011 Dermatology Online Journal