Familial benign pemphigus
Published Web Location
https://doi.org/10.5070/D31vm603hmMain Content
Familial benign pemphigus
Thomas Casey Gallagher, M.D.
Dermatology Online Journal 6(1): 7
Department of Dermatology, New York UniversityPATIENT: 38-year-old man
DURATION: Thirty-one years
DISTRIBUTION: Lateral aspects of the neck and right axilla
HISTORY: The lesions have recurred and remitted since childhood. He notes pruritus with a flare of his condition. Friction seems to exacerbate the eruption. There is a history of recurrent infections. Family history includes two siblings and a paternal uncle with the same condition.
 |  |
| Figure 1 | Figure 2 |
|---|
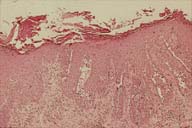
PHYSICAL EXAMINATION: Erythematous plaques with multiple, crusted erosions were noted in the right axilla and on the lateral aspects of the neck. There were no intact vesicles or bullae.
LABORATORY DATA: . None
HISTOPATHOLOGY: There is epidermal hyperplasia with areas of nearly full-thickness suprabasal acantholysis.
DIAGNOSIS: Familial benign pemphigus
COMMENT: Familial benign pemphigus, which is known as Hailey-Hailey disease, is an autosomal dominant condition that arises from a disorder in keratinocyte adhesion.[1] Skin fragility is probably due to abnormalities in desmosomal components and keratin filament attachment to desmosomes.[2,3,4] Skin infections with yeast, bacteria, and viruses may play a role in the pathogenesis. Both sexes are equally affected.
Although onset in childhood has been reported, signs and symptoms of familial benign pemphigus characteristically appear after age eleven, with most lesions developing in the third or fourth decade.[5] The majority of patients have limited involvement, which primarily affects the axillae, groin, intertrigenous folds, and posterior neck. Mucosal surfaces are rarely affected. Longitudinal white streaks of the nail plate occur in up to one-half of patients.
Most patients report no related health problems but occasionally complain that their affected skin is malodorous. Many patients note an exacerbation of their condition with friction. Others note worsening after sun exposure.
The differential diagnosis includes intertrigo and chronic bacterial and fungal infections. While pemphigus vulgaris may clinically resemble familial benign pemphigus, it typically is more widespread and often affects the mucosae. Histologic changes are characteristic and useful for establishing the diagnosis.
Familial benign pemphigus often responds to topical or systemic antimicrobial agents. Topical tetracycline, fusidic acid, and imidazole preparations have proved useful. Systemically, the tetracyclines have provided the best results. Oral glucocorticoids should be reserved for the most severe cases, as a rebound phenomenon may occur with withdrawal. One series advocated a combination of topical or systemic antimicrobials and topical glucocorticoids. Many other treatments have proved useful in the treatment of familial benign pemphigus and include methotrexate, retinoids, cyclosporine, Grenz rays and carbon dioxide laser.[6]
References
1. Marsch WC; Stuttgen G. Generalized Hailey-Hailey disease. British Journal of Dermatology, 1978 Nov, 99(5):553-60 PubMed.2. Ishibashi Y; Kajiwara Y; Andoh I; Inoue Y; Kukita A. The nature and pathogenesis of dyskeratosis in Hailey-Haileyís disease and Darierís disease. Journal of Dermatology, 1984 Aug, 11(4):335-53 PubMed.
3. Haftek M; Kowalewski C; Mesnil M; Blaszczyk M; Schmitt D. Internalization of gap junctions in benign familial pemphigus (Hailey-Hailey disease) and follicularis (Darierís disease). British Journal of Dermatology, 1999 Aug, 141(2):224-30 PubMed.
4. McGrath JA. Hereditary diseases of desmosomes. Journal of Dermatological Science, 1999 Jun, 20(2):85-91 PubMed.
5. Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. British Journal of Dermatology, 1992 Mar, 126(3):275-82 PubMed.
6. Kruppa A; Korge B; Lasch J; Scharffetter-Kochanek K; Hunzelmann N. Successful treatment of Hailey-Hailey disease with a scanned carbon dioxide laser [letter] . Acta Dermato-Venereologica, 2000 Jan-Feb, 80(1):53-4 PubMed.
© 2000 Dermatology OnLine Journal

