Unilateral colloid milium: A rare presentation
Published Web Location
https://doi.org/10.5070/D31h11c8bhMain Content
Unilateral colloid milium: A rare presentation
Parviz Toossi MD1, Safoura Shakoei MD1, Somayeh Hejazi MD1, Zahra Asadi MD2, Maryam Yousefi MD1
Dermatology Online Journal 17 (3): 6
1. Department of Dermatology, Skin Research Center, Shahid Beheshti University of MedicalSciences, Tehran, Iran. myousefi_md@yahoo.com2. Department of Dermatopathology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Abstract
We report a case of a 31-year-old man with asymptomatic papules on one side of his face that had been present for 31 months. On physical examination, he had clusters of 1 to 4 mm skin colored translucent and dome-shaped, papules forming a plaque with a size of 4 x 3 cm on his left mandibular angle. Histopathology revealed atrophy of the epidermis with extensive deposition of pale eosinophilic homogenous deposits containing artifactual fissures that were PAS positive, diastase resistant, and Congo red negative. The final diagnosis was unilateral colloid milium.
Introduction
Colloid milium (CM) is a rare cutaneous condition of uncertain etiology characterized by translucent papules on sun-exposed regions that include the face, neck, and dorsal aspects of the hands and back. Several etiologies have been postulated including chronic exposure to UV light, contact with petroleum products, application of bleaching creams containing hydroquinone, and genetic predisposition [1]. Three variants of CM are: an adult-onset type [2], juvenile form [3], and nodular colloid degeneration [2]. We report a 31-year-old man with adult onset colloid milia on his face.
Case Report
A 31-year-old man was referred to our clinic for asymptomatic papules on one side of his face that had been present for 31 months.
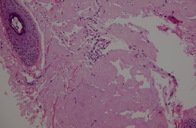
 |
| Figure 1 |
|---|
On physical examination, he had clusters of 1 to 4 mm skin colored translucent and dome-shaped, papules, forming a plaque with a size of 4 x 3 cm on his left mandibular angle (Figure 1). His skin type was III according to Fitzpatrick classification. The eruption had been noted by the family for the past 31 months, during which time the papules had gradually increased in both number and extent. His skin was otherwise normal. He had no other current or past medical problems. His medical history was negative for photosensitizing medications and disorders. There was no family history of similar skin problems in his parents or siblings. He mentioned no occupational exposure to chemicals and he had no long-term exposure to sunlight. The patient had previously been treated with topical retinoids and cryosurgery, without marked improvement. A biopsy was taken from one of his lesions with the clinical differential diagnoses of lymphangioma and steatocystoma multiplex.
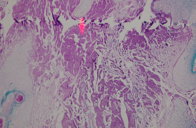
 | 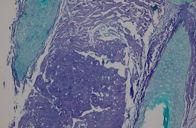 |
| Figure 2 | Figure 3 |
|---|
 |
| Figure 4 |
|---|
Histologic exam by Hematoxylin and Eosin staining revealed partial atrophy of the epidermis with extensive deposition of pale eosinophilic homogenous material containing artifactual fissures. There was also a mild infiltration of mononuclear inflammatory cells including lymphocytes, rare plasma cells, and mast cells, mostly around blood vessels of the superficial dermis (Figure 2).The amorphous deposits were crystal violet negative, PAS positive, and diastase resistant (Figures 3 and 4). Staining with Congo red was also negative.
Discussion
Colloid milium is a rare clinical entity whose true incidence is unknown because people with milder forms may not seek medical attention. Colloid milium was first described by Wagner in 1866 as “Das Colloid-Milium der Haut” and has been known historically as colloid pseudomillium, colloid infiltration, milliary colloidoma, hyaloma, and elastosis colloidalis conglomerate [2, 4].
There are three clinical types: adult form, juvenile form, and nodular colloid degeneration.
The adult form can be considered as a consequence of excessive exposure to sun, petroleum constituents, hydroquinone, and chemical fertilizers [5]. It has been reported in oil refinery workers [1]. Holzberger et al reported 28 CM in a group of workers employed in an oil refinery in the tropics who had used “gas-oil” to clean their hands [6].
The juvenile form is inherited and presents before puberty. It is probable that this variant is a result of an inherited susceptibility to ultraviolet (UV) light and can be transmitted in both an autosomal recessive and an autosomal dominant manner [7, 8, 9].
Nodular colloid degeneration has also been classified as a variant of nodular amyloidosis. The disorder most commonly presents as an isolated nodule on the face, trunk, or scalp and may be up to 5 cm in size [1].
The face, periorbital region, backs of the hands, back and sides of the neck, and ears are the most common sites of involvement. The lesions are characterized clinically by clusters of 1 to 5 mm yellowish or gray-white shiny papules or dome-shaped nodules; they are firm to the touch. Stroking may induce purpura in the lesions of colloid millium. Usually there is no associated systemic abnormality [10].
By light microscopy, colloid milium is found in the middle and upper dermis and is characterized by accumulation of a homogeneous, amorphous, faintly eosinophilic material with cleft-like spaces. The colloid masses also contain spindle and stellate shaped fibroblasts arranged along the lines of clefts. The overlying epidermis is intact and may be hyperkeratotic or flattened. Actinic changes, such as solar elastosis, may be found in close proximity to the colloid with normal elastic fibers clumped in between the colloid and the epidermis [11].
The differential diagnosis of CM may include lichen amyloidosus, milium, syringomas, steatocystoma multiplex, lipoid proteinosis, retention cysts, sarcoidosis, molluscum contagiosum, papular mucinosis, and senile sebaceous hyperplasia. Systemic amyloidosis (SM) and primary cutaneous amyloidosis may be confused with CM both on clinical and on histopathological grounds [12, 13].
Besides the case presented here, there are only 5 other cases of unilateral adult onset colloid milium in the literature. In 1972 Hashimoto et al described a 46-year-old taxi driver with colloid milium on the cheeks and the dorsum of the hands but more severe involvment of the left side, which had more long-term exposure to the sun.
Also 2 cases of unilateral colloid milium in taxi drivers (who drove their vehicles with their left arms propped out of the window exposed to the sun [14]) have been reported. An additional case was a truck driver who had similar lesions on his arm for many years [1].
Those 4 cases described above, support a relationship between long-term sun exposure and adult colloid milium. But only one case of unilateral colloid milium with no long-term sun exposure and occupational exposure to chemicals has ever been described. That was a 59-year-old woman with a 9-month history of itchy multiple papules on a non-sun-exposed area, the inner aspect of the right ear. She had no known family history of colloid milium. No occupational exposure to chemicals could be illicited in that patient either [1]. Our case was also unusual in that it was unilateral and no predisposing factors such as car exposure to sunlight were present.
References
1. Lim C, Li M. Colloid milium arising on a non-sun-exposed area in an adult. Australas J Dermatol. 2006 May; 47(2):137-8. [PubMed].2. Christie T, Joseph M, George J, Hruza G. Adult-Onset Facial Colloid Milium Successfully Treated with the Long-Pulsed Er:YAG Laser. Dermatol Surg 2002 Mar; 28(3): 215-219. [PubMed].
3. Chowdhury M, Blackford S, Williams S. Juvenile colloid milium associated with ligneous conjunctivitis: report of a case and review of the literature. Clin Exp Dermatol 2000 mar; 25(2): 138-140. [PubMed].
4. Innocenzi D, Barduagni F, Cerio R, Wolter M. UV-induced colloid milium. Clin Exp Dermatol 1993 Jul; 18(4):347-50. [PubMed]
5. Gonul M, Cakmak S, Kilic A, Gul U, Heper A. Pigmented coalescing papules on the dorsa of the hands: pigmented colloid milium associated with exogenous ochronosis. J Dermatol 2006 Apr; 33(4): 287-90. [PubMed].
6. Muscardin L, Bellocci M, Balus L. Papuloverrucous colloid milium: an occupational variant. British Journal of Dermatology.2000 Oct; 143(4): 884-887. [PubMed].
7. Touart D, Sau P. Cutaneous deposition diseases. Part I. J Am Acad Dermatol 1998Aug; 39(2): 149.-71. [PubMed].
8. Hashimoto K, Nakayama H, Chimenti S, et al. Juvenile colloid milium. Immunohistochemical and ultrastructural studies. J Cutan Pathol 1989 Jun; 16(3): 164-174. [PubMed].
9. Handfield J, Atherton D, Black M, Hashimoto K, McKee P. Juvenile colloid milium: clinical, histological and ultrastructural features. J Cutan Pathol 1992 Oct; 19(5): 434-8. [PubMed].
10. Muzaffa W, Rashid Dar N, Majeed Malik A. Colloid Milium of the Upper Eyelid Margins. Ophthalmology, 2002 Oct; 109(10):1944-1946. [PubMed].
11. Lewis A, Le E, Quan L, Krishnan B, Schulmeier J, Hsu S. Unilateral colloid milium of the arm. J. Am. Acad. Dermatol.2002Feb; 46(2): S5-7. [PubMed].
12. Giordano G, Ricci R, Froio E, Izzi G, Barone A, Boccaletti V. A case of colloid milium in patient with beta thalassaemia major. J Cutan Pathol 2008 Jun; 35(6): 566-569. [PubMed].
13. Kirtak N, Serhat Inaloz H, Karakok M, Ozgoztasi O. A case of adult colloid milium with chronic sun exposure. International Journal of Dermatology 2002Dec; 41(12): 933-936. [PubMed].
14. Fern E, Peter B. Unilateral colloid milium 1990 Dec; 23 (6 Part 1):1166-7. [PubMed].
© 2011 Dermatology Online Journal

