Patients are happy to be informed of their final non-melanoma skin cancer results by post
Published Web Location
https://doi.org/10.5070/D317h704kvMain Content
Patients are happy to be informed of their final non-melanoma skin cancer results by post
Penelope Thomson MD, Ioulios Palamaras MD, Virginia Hill MD, Wanda Robles MD PhD, Howard Stevens MD PhD
Dermatology Online Journal 16 (1): 5
Barnet & Chase Farm NHS Hospitals Trust, Herts, London, United Kingdom. drioulios@hotmail.comAbstract
During the past year, because of increasing pressure to see more patients, we have started to write to our patients informing them in a letter of their final skin cancer histology results following surgery for non-melanoma skin cancers: basal cell carcinoma and squamous cell carcinoma only. A questionnaire-based study was carried out to assess whether patients were happy to receive information concerning their non-melanoma skin cancer diagnosis in a carefully worded letter. One-hundred fifty patients were involved with a diagnosis of "completely excised non-melanoma skin cancer (NMSC)" that had previously received their final diagnosis by post. Seventy-seven (51.3%) patients responded to the questionnaire. Eighty-seven percent felt that they had been given the cancer diagnosis in an appropriate manner; 90 percent reported that they had understood the explanation about their skin cancer. In addition, 81 percent stated that they had been sufficiently involved in the discussion about their skin cancer and its treatment. Patients gave an average rating of 7.76 (1 = poor and 10 = excellent) for the overall experience of care that they had received. By writing to the patient with their final histology results, we have reduced the number of follow-up appointments without reducing the quality of patient care.
Introduction
During the past year, because of the increasing demand to see more patients, we have started to write to our patients informing them in a letter of their final skin cancer histology results following surgery for non-melanoma skin cancers (NMSC): Basal cell carcinoma (BCC) and Squamous cell carcinoma (SCC), only.
In Barnet and Chase Farm Hospitals, it is common practice to discuss the likelihood of a NMSC diagnosis with the patient several times before the final histology result becomes available, at first consultation and booking of the surgical procedure and at the time of the surgical procedure.
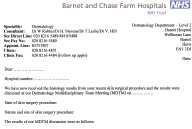 |
| Figure 1 |
|---|
Our surgical practice is to perform a diagnostic biopsy for most skin lesions when we are suspicious of skin cancer. Following a discussion on the histology results at our Local Multidisciplinary Team Meeting (LMDT), a letter is sent to the patient by post on that same day in which we inform the patient of the result and invite them to return for the definitive surgical procedure. However, some lesions are small and because of the long biopsy waiting lists, these are excised directly. When the histology result is available we write to the patient informing them of the latter (Figure 1), The letter relates LMDT's decision and encloses both the relevant British Association of Dermatologists patient information sheet (for BCC and SCC) [1, 2] and key worker's contact details in case the patients want to discuss their results in person.
Patients with a diagnosis of a completely excised BCC are not seen in the clinic again after their tumor has been removed and are followed up by their family physician. Patients with a completely excised SCC are invited to one further clinic appointment for review after the letter informing them of the diagnosis has been sent to them. Of note, we always give patients with a melanoma diagnosis or other malignant skin tumor diagnosis their results in a face-to-face consultation.
Methods
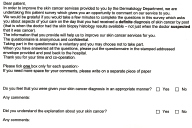 |
| Figure 2 |
|---|
A letter with an accompanying questionnaire (Figure 2) was sent to all the patients (n=150) who were given a diagnosis of a "completely excised NMSC" over a three-month period (from February 2, 2009 to May 1, 2009), giving a representative sample of our NMSC population.
Results
Seventy-seven (51.3%) patients responded to the questionnaire. Based on the results obtained from the completed questionnaires, 87 percent felt that they had been given the cancer diagnosis in an appropriate manner; 90 percent reported that they had understood the explanation about their skin cancer and 81 percent stated that they had been sufficiently involved in the discussion about their skin cancer and its treatment.
In addition, when asked how they rated their experience of the care that they received when given their skin cancer diagnosis, patients gave an average rating of 7.76 (1 = poor and 10 = excellent).
Conclusions
Communication between doctors and patients is an essential aspect of cancer care, particularly when giving the patient the diagnosis of skin cancer. There has been extensive research into how to break bad news to patients and concerning patients' preferences regarding communication of cancer diagnoses [3, 4, 5, 6]. There has been only one study about melanoma patients, in which 131 newly diagnosed melanoma patients were asked with a posted questionnaire to document their satisfaction of their communication with the physician for their initial diagnosis [7]. Of these, 62 percent favored a face-to-face consultation. To our knowledge there have been no studies assessing how patients would prefer to receive a diagnosis of a non-melanoma skin cancer.
In all studies, a face-to-face consultation between a health-care professional and the patients is the favored way of breaking cancer news [3].
Our results suggest that patients are happy to receive information concerning their non-melanoma skin cancer diagnosis in a carefully worded letter accompanied by an appropriate information leaflet containing consistent and nationally agreed upon information regarding the nature and prognosis of their NMSC. Of note, a previous study has shown that melanoma patients also value written information about their diagnosis [7].
By writing to the patient with their final histology results, we have reduced the number of follow-up appointments without reducing the quality of patient care.
References
1. British Association of Dermatologists website: Basal cell carcinoma information sheet. (last accessed on 08/27/2009)2. British Association of Dermatologists website: Squamous cell carcinoma information sheet. (last accessed on 08/27/2009)
3. Fujimori M, Uchitomi Y. Preferences of cancer patients regarding communication of bad news: a systematic literature review. Jpn J Clin Oncol. 2009; 39(4):201-16. Epub 2009 Feb 3. [PubMed]
4. Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet. 2004 Jan 24; 363(9405):312-9. [PubMed]
5. Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP, Spikes A. A Six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000; 5(4):302-11 [PubMed]
6. Girgis A, Sanson-Fisher RW. Breaking bad news. 1: Current best advice for clinicians. Behav Med. 1998; 24(2):53-9. [PubMed]
7. Schofield PE, Beeney LJ, Thompson JF, Butow PN, Tattersall MH, Dunn SM Hearing the bad news of a cancer diagnosis: the Australian melanoma patient's perspective. Ann Oncol. 2001; 2(3):365-71. [PubMed]
© 2010 Dermatology Online Journal

