Irritant contact dermatitis from exposure to povidone-iodine may resemble toxic epidermal necrolysis
Published Web Location
https://doi.org/10.5070/D314h5d8wqMain Content
Irritant contact dermatitis from exposure to povidone-iodine may resemble toxic epidermal necrolysis
Travis W Vandergriff MD1, Carina A Wasko MD1, Mary R Schwartz MD2, Sylvia Hsu MD1
Dermatology Online Journal 12 (7): 12
1. Department of Dermatology, Baylor College of Medicine 2. Department of Pathology, The Methodist Hospital, Houston, Texas
Irritant contact dermatitis (ICD) should be considered in the differential diagnosis of blistering skin eruptions and epidermal necrosis in patients with a history of exposure to povidone-iodine solution. The skin lesions of ICD may clinically and histologically resemble the lesions of toxic epidermal necrolysis (TEN), creating the potential for confusion between the two diagnoses.
Clinical synopsis
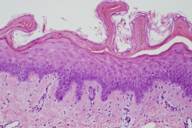
A dermatology consult was requested for a 66-year-old woman who developed erythema and a bullous eruption in the axillae and abdominal folds after undergoing aortic valve replacement and ascending aortic aneurysm repair. Her chest and upper abdomen were prepared with 10 percent povidone-iodine solution pre-operatively. Immediately post-operatively she noticed a burning pain in the axillae and abdominal folds. Within 24 hours she had developed a well-marginated, erythematous blistering eruption confined to the skin folds at these sites; she soon developed epidermal necrosis with sloughing of the involved skin (Fig. 1). There was no mucous membrane involvement. Histopathologically, the lesions showed full-thickness epidermal necrosis with underlying epidermal regeneration, mild spongiosis, and focal scant perivascular inflammatory infiltrates (Fig. 2). In this case, prolonged exposure to 10% povidone-iodine solution, which drained to dependent areas and settled in the skin folds, produced a severe irritant contact dermatitis resulting in necrosis.
Comment
In ICD the epidermal damage occurs because of a direct effect of the toxic agent on keratinocytes [1]. The irritant substances are thought to result in epidermal damage by denaturing keratin proteins, removing lipid compounds, and directly interacting with cell membranes [2]. There is no immunologically mediated component to ICD, although individuals with atopic dermatitis are more likely to develop ICD when exposed to an irritant [3]. Commonly implicated irritants include corrosive materials, alkalis, acids, organic solvents, detergents, and disinfectants. Different irritant compounds can produce different clinical manifestations, ranging from erythema to erosions, blistering, and overt necrosis. Even the histopathology of ICD can vary by the cause, with some irritants demonstrating unique characteristic findings on tissue biopsy [1]. For example, exposure to the irritant dithranol typically leads to balloon degeneration of the upper dermis while sodium lauryl sulfate characteristically causes parakeratosis and intracytoplasmic vesiculation [1].
Povidone-iodine solution, commercially available as Betadine® Microbicide, is a relatively uncommon but recognized cause of ICD [4, 5, 6]. The 10-percent solution, a commonly used surgical antiseptic, contains povidone (polyvinylpyrrolidone) and 1 percent available iodine. The solution has microbicidal activity against a broad spectrum of organisms, including bacteria, viruses, and fungi [7]. Its microbicidal effect is achieved minutes after application as the iodide ion interacts with the microbial cell membrane [7]. Reported cases of ICD caused by povidone-iodine solution have appeared within 2 days of exposure and have manifested as erythematous bullae, erosions, and eventual necrosis in a clearly marginated distribution corresponding to the areas of exposure to the solution [4, 5, 6]. Many of the lesions of ICD attributed to povidone-iodine solution have been described as chemical burns [4, 5].
The reported skin findings of ICD from povidone-iodine solution resemble those of TEN both clinically and histopathologically. Like severe ICD, TEN typically begins as a painful burning sensation followed by an erythematous and edematous eruption. Large sections of the epidermis then slough in sheets, accompanied by full thickness epidermal necrosis [8]. Irritant contact dermatitis may resemble TEN on tissue biopsy as well. Microscopically, TEN typically shows complete necrosis of the epidermis with subepidermal blisters, a sparse mononuclear infiltrate, basalar vacuolization, and mild spongiosis [9].
Although TEN and severe ICD share many clinical and histopathological findings, distinguishing between the two entities may be possible by careful history and physical examination. A history of exposure to a known irritant, with symptoms appearing within hours to days of exposure, suggests the diagnosis of ICD [7]. A historical link between an immunocompromised state and skin sensitivity to povidone-iodine solution has also been proposed [10]. Unlike ICD, most cases of TEN are associated with reaction to a medication. Symptoms begin on average 2 weeks after exposure to the offending agent. Commonly implicated drugs include sulfonamides, anticonvulsants, non-steroidal anti-inflammatory drugs, and allopurinol [8]. On physical examination, ICD may appear as erythematous, fissured, and blistered, with a glazed or scalded skin [7]. The diagnosis of ICD is strongly supported when lesional skin is restricted to geometric distributions suggestive of an exogenous, rather than endogenous, cause. In this case, the clue to diagnosis is the linear streaking pattern from the running solution. These types of patterns will often identify that there is an external cause. Evidence of gravitational influence on the distribution of lesional skin, such as confinement to dependent areas or restriction to skin folds, is also strongly supportive of the diagnosis of ICD [7]. Unless the mucous membranes were exposed to the irritant compound, they will not be involved in ICD. Conversely, mucous membranes are almost invariably involved in TEN [8]. The lesional skin of TEN does not typically demonstrate a clearly marginated geographic distribution.
As in any case of contact dermatitis, patients with ICD should avoid exposure to the offending agent. Barrier creams, such as those containing 5-percent perfluoropolyether or dimethicone lotion, may be effective in preventing or abating ICD, should the patient come in contact with the irritant compound in the future [11]. The mainstay of treatment for ICD is irritant withdrawal and avoidance and topical application of lipid rich moisturizers [11]. Topical corticosteroids should be used cautiously in patients with ICD because these agents may lead to epidermal atrophy, increasing skin fragility, and vulnerability to additional irritation [11].
References
1. Rietschel RL, Fowler JF Jr. Fisher's Contact Dermatitis. 4th ed. Baltimore, MD: Williams & Wilkins, 1995: 39, 330.2. Rietschel RL. Clues to an accurate diagnosis of contact dermatitis. Dermatol Ther 2004;17:224-230.. Wahlberg JE. “Clinical Overview of Irritant Dermatitis.” 3. The Irritant Contact Dermatitis Syndrome. Eds. van der Valk PGM, Maibach HI. New York: CRC Press, 1996: 1-6.
4. Iijima S, Kuramochi M. Investigation of irritant skin reaction by 10% povidone-iodine solution after surgery. Dermatology 2002;204:103-108.
5. Corazza M, Bulciolu G, Spisani L, Virgili A. Chemical burns following irritant contact with povidone-iodine. Contact Dermatitis 1997;36:115-116.
6. Okano M: Irritant contact dermatitis caused by povidone-iodine. J Am Acad Dermatol 1989;5:860.
7. Zamora JL. Chemical and microbiologic characteristics and toxicity of povidone-iodine solutions. Am J Surg 1986;151:400-406.
8. Roujeau JC, Chosidow O, Saiag P, Guillaume JC. Toxic epidermal necrolysis (Lyell syndrome). J Am Acad Dermatol 1990;23:1039-1058.
9. Paquet P, Pierard GE. Erythema multiforme and toxic epidermal necrolysis: a comparative study. Am J Dermatopathol 1997;19:127-132.
10. Feldtman RW, Andrassy RJ, Page CP. Povidone iodine skin sensitivity observed with possibly altered immune status. JAMA 1979;242:239.
11. Saary J, Qureshi R, Palda V, DeKoven J, Pratt M, Skotnicki-Grant S, Holness L. A systematic review of contact dermatitis treatment and prevention. J Am Acad Dermatol 2005;53:845.e1-845.e13.
© 2006 Dermatology Online Journal