Trichophyton raubitschekii: A new agent of dermatophytosis in Brazil?
Published Web Location
https://doi.org/10.5070/D312x9h4m6Main Content
Trichophyton raubitschekii: A new agent of dermatophytosis in Brazil?
A R Costa1, P R Criado1, N Y S Valente1,2, J A S Sittart1, R S Stelmach1 and C Vasconcellos1,3
Dermatology Online Journal 9 (1): 6
1. Medical Mycology Laboratory. Dermatology Unit. Hospital do Servidor Publico Estadual de Sao Paulo, SP Brazil, 2. LIM53
-HC-FMUSP, 3. LIM72 -HC-FMUSP, BrazilAbstract
A microbiological and ultrastructural study of Trichophyton raubitschekii recovered from a patient with tinea faciei is presented. This is the second case of isolation of this fungus in Sao Paulo and the sixth case in Brazil. Upon culture, the morphological pattern and the physiological tests performed confirmed the identification of T. raubitschekii. The ultrastructural study of T. raubitschekii showed the presence of a membrane-like structure located in the outer portion of the hyphal walls. This structure was bi-stratified and very like the one observed in T. rubrum. Is T. raubitschekii a new fungus emerging in Brazil or is it a T. rubrum variant?
Introduction
T. raubitschekii was reported as a new species by Kane et al.[1] It is a dermatophyte with similarities to both T. rubrum (Cast) Sabouraud and T. mentagrophytes (Robin) Blanch.
Kane et al.[2] studied 38 cases of this infection and published data showing the usual preponderance of males (2:1) and high proportion (60.5%) of individuals of Asian origin among the cases. Out of thirty-eight patients surveyed, twenty-three had previous Asian residence. Of these, seven were from China, Vietnam, Hong Kong, North India, Pakistan, and the Middle East. Among the non-Asian patients, seven originated from South Europe (Portugal, Spain, Italy or Greece) and eight reported previous North or East European, or exclusive North American residence. Infection with this fungus usually manifests as tinea corporis, but may also cause tinea pedis, tinea cruris and tinea unguium. One case of tinea capitis has been reported.[2] In Brazil, T. raubitschekii was isolated for the first time from four Rio de Janeiro patients.[3] They had typical tinea corporis lesions. Out of nine hundred forty-five dermatophyte isolates by the authors, from November 1992 to April 1994, only four (0.42%) were of T. raubitschekii.[3] After these cases, no more cases were reported in Brazil up to 1999, when the first case in Sao Paulo was diagnosed.[4]
Case Report
Subject
ASM, a 49 year-old female, born and living in city of Diadema (Sao Paulo), presented with papulo-erythematous and slightly pruritic lesions on the left side of the face (Figure 1).
 |
| Figure 1 |
|---|
| Fig 1: Tinea faciei (clinical feature): Erythematous plaque, slight scaling, poorly defined on the left malar prominence. |
The patient had been treated elsewhere for chronic cutaneous lupus erythematosus (lupus tumidus) without improvement. After mycological direct exam and culture of the material obtained by a scraping of the skin lesion, the diagnosis of tinea faciei caused by T. raubitschekii was achieved. The patient was properly treated with an antifungal agent producing a clinical and mycological cure.
Techniques
The dermatophyte cultures were made on Sabouraud 2% Glucose Agar (DIFCO), with cloramphenicol 0,05% and cycloheximide 0,5%, for ten days at 25oC.
Physiological tests were performed in Christensen urea broth, bromocresol purple casein agar (BPCA) and Sabouraud-peptone-glucose agar (SPGA) with 5% sodium chloride.[2,5,6]
- Micromorphological study by slide culture was performed.
- A small part of the colony was fixed in glutaraldehyde and processed for transmission electron microscopy (TEM).[7]
- Skin sample was fixed in 10% buffered formalin solution, embedded in paraffin, sectioned (6m) and stained with hematoxylin-eosin (HE).
Results
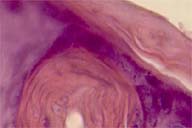
Histopathologic exam displayed hyphae among ortho and parakeratotic keratinocytes of the folicular infundibulum, which also exhibited spongiosis and exocytosis of lymphocytes (Figure 2). There were also a few mononuclear cells around superficial perifollicular dermal vessels.
After ten days of culture at 25oC there was a deep red purple, subglabrous fungus colony which, after twenty days, became wrinkled and granular on the surface.
Microscopic examination of the culture revealed numerous cylindrical to pencil shaped macroconidia and subglobose to pyriform or clavate microconidia. Both macroconidia and microconidia were abundant (Figure 3).
The results of physiological tests performed were: 1.seven days to hydrolyse urea in Christensen urea broth 2.failure to produce alkaline substances on BPCA medium after seven days of incubation at 25oC 3.restriction of growth on SPGA medium with 5% sodium chloride.
The morphological pattern and the physiological tests performed confirmed the identification of T. raubitschekii.[3]
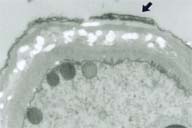
Transmission electronic microscopy(TEM) of the culture showed morphological findings similar to that described for T. Rubrum.[8] Under TEM, the ultrastructural study of T. raubitschekii showed the presence of a membrane-like structure located in the outer portion of the wall of the hyphae, which was bi-stratified (Fig 4), as observed by Mares et al. on ultrastructural study of T. rubrum.[8]
 |
| Figure 4 |
|---|
| Fig 4: Trichophyton raubitschekii (transmission electron microscopy): Membrane-like structure (arrow) in the outer part of the bi-stratified hyphaes wall (OM 9500x). |
Discussion
Although T. raubitschekii shares taxonomic similarities to the more common T. rubrum group, it shows some differences in clinical and laboratory features. The majority of patients until now reported, originated from or had lived in one of the South or East Asian countries where the organism may be endemic or sporadic.[2] Inflammatory lesions are often seen, as in our case.
According to Summerbell & Kane T. raubitschekii colonies can be similar to T. violaceum or T. rubrum and T. mentagrophytes.[9] Our colonies resembled T. violaceum.
An interesting finding was that by TEM there was a membrane-like, bi-stratified layer structure located in the outer portion of the hyphae wall, similar to that previously described for T. Rubrum.[8] Its presence demonstrates ultrastructural, morphological similarity between T. rubrum and T. raubitschekii. However, T. rubrum and T. raubitschekii have some morphological, physiological, and ecological distinctions. Therefore, the retention of current phylogenetic species status requires further evaluation.[10]
Recently, Kano et al. analyzed nucleotide sequences of the chitin synthase 1 (CHS1) gene for the evaluation of the phylogenetic relationship between T. violaceum and T. rubrum.[11] The study included two isolates of T. raubitschekii and one isolate of T. rubrum var. nigricans. This study showed that two strains of T. raubitschekii and one isolate of T. rubrum var. nigricans shared more than 98% of their nucleotide sequences with T. rubrum, indicating that they could be classified in the same species.
Conclusion
T. rubrum is the most common causative agent of dermatophytosis in Brazil.[12] Nevertheless, T. raubitschekii could be misdiagnosed and taken as T. rubrum or as T. mentagrophytes. It remains unclear whether T. raubitscheki is really a new species of fungus emerging in Brazil or a T. rubrum variant.
Acknowledgements: We are grateful to Dr. N. Takahashi de Melo and E.M. Heins-Vaccari, Instituto de Medicina Tropical de Sao Paulo to confirming our mycological findings and W. M. Maranhao for technical assistance.
References
1 Kane J, Salkin IF, Weitzman I, Smitka C, Trichophyton raubitschekii sp. nov. Mycotaxon 1981;13:259-266.2 Kane J, Krajden S, Summerbell RC, Sibbald RG, Infections caused by Trichophyton raubitschekii: clinical and epidemiological features. Mycosis 1990;33:499-506.
3 Caiuby MG, Monteiro PCF, Nishikawa MM, Isolation of Trichophyton raubitschekii in Rio de Janeiro (Brazil). J Med Vet Mycol 1996;34: 361-363.
4 Lacaz CS, Zaitz C, Ruiz LRB, Souza VM, Santos, ARA, Muramatu LA, Melo NT, Heins-Vaccari EM, Fernndez-Arriagada GL, Freita-Leite RS, Dermatophytosis caused by Trichophyton raubitschekii, Report of the first case in Sao Paulo, Brazil. Rev Inst Med Trop S Paulo 1999;41(5):313-317.
5 Kane J, Fisher JB, The differentiation of Trichophyton rubrum and Trichophyton mentagrophytes by use of Christensen's urea broth. Can J Microbiol 1971;17:911-913.
6 Kane J, Fisher JB, The effect of sodium chloride on the growth and morphology of dermatophytes and some other keratolytic fungi. Can J Microbiol 1975;21:742-749.
7 Duarte MIS, Mariano OM, Takakura CFH, Uip DE, Corbett CEP, A fast method for processing biologic material for electron microscopy diagnosis in infectious disease. Ultrastruct Pathol 1992;16:475-482.
8 Mares D, Romagnoli C, Sacchetti G, Vicentini CB, Bruni A, Morphological study of Trichophyton rubrum: ultrastructural findings after treatment with 4-amino-3-methyl-l-phenyl-pyrazolo-(3,4-c) isothiazole. Med Mycology 1998;36:379-385.
9 Summerbell RC, Kane J, The genera Trichophyton and Epidermophyton in Laboratory handbook of dermatophytes. A clinical guide and laboratory handbook of fungi from skin, hair and nails. ed. Kane J, Summerbell RC, Krajden S, Sigler L, Land G, Belmont, 1997.
10 Summerbell RC, Haugland RA, Li A, Gupta AK, rRNA gene internal transcribed spacer 1 and 2 sequences of asexual anthropophilic dermatophytes related to Trichophyton rubrum. J Clin Microbiol 1999;37(12):4005-4011.
11 Kano R, Okabayashi K, Nakamura Y, Ooka S, Kashima M, Mizoguchi M, Differences among chitin synthase I gene sequences in Trichophyton violaceum and T. rubrum. Med Mycol 2000;38(1):47-50.
12 Lacaz CS, Porto E, Martins JEC, Micoses Superficiais in Micologia medica. ed.Lacaz CS, Porto E, Martins JEC,1991.
© 2003 Dermatology Online Journal