Skin metastasis of head and neck carcinoma predictive for dismal outcome
Published Web Location
https://doi.org/10.5070/D30z5143r2Main Content
Skin metastasis of head and neck carcinoma predictive for dismal outcome
J Thariat MD1, C BadoualMD2, S Hans MD PhD3, T Meatchi MD2, M Housset MD1
Dermatology Online Journal 14 (6): 8
1. Department of Radiation Oncology, Hôpital Européen Georges Pompidou, Paris, France. jthariat@hotmail.com2. Department of Pathology, Hôpital Européen Georges Pompidou, Paris, France
3. Department of Otorhinolaryngology and Head and Neck Surgery, Hôpital Européen Georges Pompidou, Paris, France
Abstract
A 64-year-old female with locally advanced oropharyngeal carcinoma presented with an innocuous appearing macule on the abdomen. The lesion rapidly enlarged over 2 weeks into an inflammatory 5 cm fleshy nodule that was diagnosed as squamous cell carcinoma (SCC) and was found to overexpress epidermal growth factor receptor (EGFR). A fatal outcome occurred 3 months after the initial diagnosis of cancer, in spite of chemotherapy and treatment with EGFR inhibitors (cetuximab). Cutaneous metastases occur in 10 percent of squamous cell carcinomas of the head and neck. Contiguous cutaneous metastases in the head and neck areas are by far the most common. Conversely, isolated infradiaphragmatic cutaneous metastases are exceedingly rare and are associated with an aggressive clinical course. In a patient with cancer, the possibility of distant skin metastasis should be considered whenever new cutaneous nodules appear.
Introduction
Cutaneous metastases occur in less than 10 percent of squamous cell carcinomas of the head and neck [1]. Stoma recurrences, permeation nodules and cutaneous metastases in the head and neck or trunk areas from nearby head and neck cancer are by far the most common. Conversely, distant cutaneous metastases to the lower part of the body are exceedingly rare in the absence of iatrogenic tumor seeding [2]. Sister Mary Joseph umbilical nodules are well known skin metastases of gastro-intestinal cancers, ovarian cancers, or lymphomas [3-5]. Very few cases of distant cutaneous head and neck SCC (HNSCC) metastases have been described [6] and are usually multiple [7]. Underreporting is likely in cases of simultaneous occurrence with lung, bone and brain metastases. Cutaneous distant metastases signify a poor prognosis and 1-year survival is 0 percent. Early diagnosis of metastases may allow a beneficial modification of the therapeutic strategy. We report the case of a solitary cutaneous metastasis from a locally advanced head and neck carcinoma. Our case illustrates the need for early recognition of distant cutaneous spread.
Report
 |
| Figure 3 |
|---|
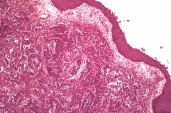
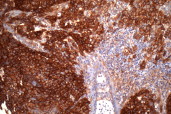
| Figure 3. Histological examination EGFR staining X20: Squamous cell carcinoma localized in the dermis and the hypodermis highly and massively stained for EGFR |
A 64-year-old female was referred to her head and neck surgeon for a 2-month history of progressive odynophagia. Endoscopy revealed a locally advanced unresectable oropharyngeal tumor centered on her left tonsil. Histological examination showed moderately-differentiated squamous cell carcinoma. On cervicothoracic computed tomography (CT) and magnetic resonance imaging (MRI) of the head and neck, her primary tumor was associated with 2 homolateral cervical metastatic nodes (TNM-AJCC 2002 stage T3N2bM0). She underwent induction chemotherapy according to multidisciplinary consensus. During her second course, 6 weeks after initial diagnosis of cancer, she reported a lump on her abdomen that had been growing from a slightly erythematous macule over the past 2 weeks. On examination, a 5 cm well-circumscribed smooth fleshy inflammatory nodule (Fig. 1) was found. The primary cancer in her tonsil was stable but metastatic nodes had increased by 20 percent. She underwent thorough evaluation prior to any further treatment. Abdominal CT showed focal subcutaneous infiltration. Positron emission tomography (PET)-CT depicted areas of hyperfixation of the 2-deoxy-2-(18) fluoro-D-glucose (FDG) in the primary tumor and nodes (SUV 5.5). It also revealed a focal uptake of the radiotracer in the abdomen, which was highly suspicious for a malignant lesion (SUV 3). Surgical excision of the lump was performed. Histology showed moderately-differentiated cells of squamous cell carcinoma permeating in groups throughout the dermis and hypodermis, as well as areas of necrosis and inflammation (Fig. 2). The overlying epidermis remained intact. Tumor cells showed severe cytonuclear atypia and mitoses. EGFR staining was highly positive in more than 90 percent of cells (Fig. 3). The patient's tonsil became painful. She therefore underwent palliative hypofractionated radiotherapy of the oropharynx associated with 4 weekly courses of the EGFR inhibitor, cetuximab. The patient died of tumor-related cachexia 3 months after the initial diagnosis and 5 weeks after the diagnosis of her cutaneous abdominal metastasis.
Discussion
The vast majority of squamous cell carcinomas of the head and neck metastasize to the lung, bone, and brain. Extension to the skin is uncommon except for contiguous involvement, including permeation nodules in the head and neck area [8]. Tumor implantation after surgical procedures [8] have also been described. However, the incidence of cutaneous metastases is probably underestimated because they are usually associated with other life-threatening metastases. Few cases of solitary distant cutaneous metastases have been described. Most lesions present as nodules or erythematous macular lesions that may mimic an infectious process [6]. Most metastases are confined to the deep dermis and spare the epidermis, but there are some cases of abutment of the epidermis or ulceration [6]. The diagnosis of a metastasis from a head and neck primary cancer is supported by the presence of a heavy dermal component that has no connection with the epidermis. Necrosis, inflammation and lymphovascular invasion can be associated. The degree of differentiation is usually the same as in the primary, although the EGFR expression may differ [9]. However, it is now commonly accepted that EGFR immunohistochemical analysis is not necessary in view of the very high rates of positive EGFR staining in head and neck cancer. In our case, patterns of differentiation and EGFR staining were similar.
There is growing evidence that K-ras [10] and PTEN status [11] can provide important information on the response to EGFR inhibitors and determine specific therapeutic schemes. Surgical excision sometimes improves the prognosis and quality of life. Our case was remarkable in 3 aspects. There was no evidence of any other systemic metastatic tumor manifestation, as demonstrated by PET-CT; local cervical nodal involvement was present. Her solitary distant metastasis was located on the abdomen and the patient had no history of surgical procedure near this site, which supports hematogenous spread as the etiology.
This report illustrates the importance of careful full examination of the skin in patients with head and neck cancer. Furthermore, this case confirmed that distant cutaneous lesions of head and neck primaries are indicative of a poor prognosis; rapid and aggressive cancer treatment is required [2, 12]. Finally, one striking feature in this case was the contrast between massive EGFR overexpression of tumor cells and the total absence of response to EGFR inhibitors. Examination for other biomarkers such as K-ras may allow treatment with combination target agents that may enhance tumor responsiveness [10].
References
1. Ferlito A, Shaha AR, Silver CE, et al. (2001) Incidence and sites of distant metastases from head and neck cancer. ORL J Otorhinolaryngol Relat Spec 63:202-207. PubMed2. Adelson RT, Ducic Y (2005) Metastatic head and neck carcinoma to a percutaneous endoscopic gastrostomy site. Head Neck 27:339-343. PubMed
3. Albano EA, Kanter J (2005) Images in clinical medicine. Sister Mary Joseph's nodule. N Engl J Med 352:1913. PubMed
4. Nagao K, Kikuchi A (1996) Images in clinical medicine. Sister Joseph's node in non-Hodgkin's lymphoma. N Engl J Med 335:1569. PubMed
5. Dodiuk-Gad R, Ziv M, Loven D, et al. (2006) Sister Mary Joseph's nodule as a presenting sign of internal malignancy. Skinmed 5:256-258. PubMed
6. Saeed S, Keehn CA, Morgan MB (2004) Cutaneous metastasis: a clinical, pathological, and immunohistochemical appraisal. J Cutan Pathol 31:419-430. PubMed
7. Krunic AL, Cockerell CJ, Truelson J, et al. (2006) Laryngeal squamous cell carcinoma with infradiaphragmatic presentation of skin metastases. Clin Exp Dermatol 31:242-244. PubMed
8. Pitman KT, Johnson JT (1999) Skin metastases from head and neck squamous cell carcinoma: incidence and impact. Head Neck 21:560-565. PubMed
9. Scartozzi M, Bearzi I, Berardi R, et al. (2004) Epidermal growth factor receptor (EGFR) status in primary colorectal tumors does not correlate with EGFR expression in related metastatic sites: implications for treatment with EGFR-targeted monoclonal antibodies. J Clin Oncol 22:4772-4778. PubMed
10. Khambata-Ford S, Garrett CR, Meropol NJ, et al. (2007) Expression of epiregulin and amphiregulin and K-ras mutation status predict disease control in metastatic colorectal cancer patients treated with cetuximab. J Clin Oncol 25:3230-3237. PubMed
11. Frattini M, Saletti P, Romagnani E, et al. (2007) PTEN loss of expression predicts cetuximab efficacy in metastatic colorectal cancer patients. Br J Cancer 97:1139-1145. PubMed
12. Cole RD, McGuirt WF (1995) Prognostic significance of skin involvement from mucosal tumors of the head and neck. Arch Otolaryngol Head Neck Surg 121:1246-1248. PubMed
© 2008 Dermatology Online Journal