Granulomatous rosacea: Unusual presentation as solitary plaque
Published Web Location
https://doi.org/10.5070/D30ws350z5Main Content
Granulomatous rosacea: Unusual presentation as solitary plaque
Mayanka Batra MD DNB, Cherry Bansal MD, Suman Tulsyan MBBS DVD
Dermatology Online Journal 17 (2): 9
Abstract
A 45-year-old male presented with a 6 month history of an enlarging smooth, erythematous plaque over the central part of his face. Mild erythema of both eyes was present. Sarcoidosis, Hansen disease, lupus vulgaris, cutaneous leishmaniasis, pseudolymphoma, foreign body granuloma, granuloma faciale, discoid lupus erythematosus, and granulomatous rosacea were considered in the differential diagnosis. CBC, urinalysis, renal function tests, liver function tests, serum electrolytes, and blood sugar were all normal. Chest X-ray and ECG revealed no abnormality. Serology for syphilis and HIV, and mantoux test were negative. Slit-skin smear, tissue smear and culture for AFB and fungi were negative. Skin biopsy revealed multiple non-caseating epitheloid granulomas around the pilosebaceous unit suggestive of granulomatous rosacea. Granulomatous rosacea, a rare entity comprising only about 10 percent of cases of rosacea can mimic many granulomatous conditions both clinically and histologically making the diagnosis an enigma. It usually presents as yellowish brown-red discrete papules on the face; non-caseating epithelioid granulomas are seen on histology examination. We herein report the case because it presented in atypical fashion, as a solitary indurated plaque on the nose, likely representing Morbihan’s disease or solid persistent facial edema of rosacea (rosacea lymphedema).
Introduction
 |  |
| Figure 1 | Figure 2 |
|---|
A 45-year-old male presented with a 6-month history of an enlarging, erythematous plaque over his nose and mid face. There was no itching. The patient reported no aggravation from sun exposure, spicy food, or alcohol. There was no history of any trauma. The patient described a history of redness of both eyes for fifteen days prior to presentation. There was no associated photophobia, foreign body sensation, dryness, or discharge. A private practitioner had treated him with topical and systemic medications without benefit. Family history and review of systems were unremarkable.
Physical Examination. A large erythematous, plaque was present over the nose extending up to the glabella. The surface was smooth and shiny without any scaling. No other part of the face or body was involved. There was no lymphadenopathy.
Ophthalmological examination. Mild conjunctival injection was present bilaterally. Vision was 6/12 in both eyes. Slit lamp and fundus examination revealed no abnormality.
Lab investigations. Complete blood count, renal function tests, liver function test, serum electrolytes, and serum calcium were within normal limits. Serology for syphilis, HIV, and ANA were negative and Mantoux test was negative. Chest X-ray and ECG were normal. Ultrasound of the abdomen revealed no abnormality. Slit skin smear, tissue smear and culture for AFB were negative. Skin scraping and culture for fungus were negative.
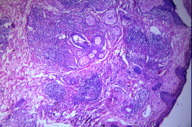
Histopathology revealed non-ceseating epitheloid granulomas with lymphohistiocytic infiltrate centered around the pilosebaceous units.
From the above investigations and histopathology, we felt we had ruled out other clinical conditions such as sarcoidosis, Hansen disease, lupus vulgaris, cutaneous leishmaniasis, pseudolymphoma, foreign body granuloma, granuloma faciale, and discoid lupus erythematosus.
The diagnosis of granulomatous rosacea was made.
Management. The patient was advised to avoid hot and spicy food, alcohol, and sun exposure. He was put on tetracycline 500mg QID and topical metronidazole gel. On follow-up after 4 weeks, our patient did not show any improvement; instead, the plaque had extended over both cheeks. isotretinoin 20mg twice daily and Prednisolone 30 mg was started and tetracycline was stopped. After 6 weeks of therapy, there was significant reduction in size of the lesion. Prednisolone was gradually withdrawn and the same dose of isotretinoin was continued for another 2 months followed by isotretinoin 20mg daily. After 3 months, the plaque had completely resolved with mild residual scarring over nose.
We report this case because granulomatous rosacea presenting as a solitary plaque is unusual. It is instructive to present the differential diagnosis and successful treatment.
Discussion
Rosacea is a chronic disorder affecting the facial convexities, characterized by frequent flushing, persistent erythema and telangiectasia, interspersed by episodes of inflammation during which swelling, papules and pustules are evident[1]. The subtypes of rosacea are erythematotelangiectatic, papulopustuar, phymatous, and ocular. Granulomatous rosacea is considered to be a part of the spectrum of rosacea and is considered as a variant of rosacea [2, 3]. It is clinically characterized by yellowish red discrete facial papules clinically; non-caseating epitheloid granulomas are observed on histology. It constitutes about 10 percent of all cases of rosacea [4]. Although the exact etiopathogenesis of GR is not known, a role of delayed hypersensitivity reaction against keratinized cells, pilosebaceous structures, and Demodex folliculorum mite has been suggested [2, 5].
Granulomatous rosacea can mimic various facial granulomatous conditions both clinically and histologically, such as lupus miliaria disseminatus faciei, micropapular sarcoidosis, and cutaneous tuberculosis [5, 6]. In our case, the main conditions in the differential diagnosis were sarcoidosis, Hansen disease, cutaneous leishmaniasis, lupus vulgaris, discoid lupus erythematosus, granuloma faciale, foreign body granuloma, and pseudolymphoma because of the unusual presentation as a solitary plaque. This type of presentation may represent Morbihan disease, also called rosacea lymphedema or solid persistent facial edema of rosacea in which granulomatous rosacea is accompanied by erythema and edema of the mid-upper third of the face [7].
Sarcoidosis is a multisystem disease defined by epitheloid cell granulomas without caseation. Cutaneous lesions range from small papules, plaques, and subcutaneous nodules to lupus pernio. Ocular findings are present in 20-30 percent of cases. The diagnosis rests on a constellation of clinical and laboratory findings. Histopathologically, there is the presence of circumscribed epitheloid cell granulomas without caseation and a sparse lymphocytic infiltrate at the periphery of the granulomas. The granulomas occur lower in the dermis than in lupus vulgaris and Hansen disease [8].
Foreign body granuloma may induce practically any pattern of granulomatous inflammation. A history of trauma with probable entry of a foreign body is usually present and the skin lesion usually progresses from ulcer to granuloma.
Lupus vulgaris typically presents as plaque formed by the coalescence of red brown papules, which have a tendency to heal slowly in one area with scarring and progress in other areas. Histopathology shows granulomas with caseation necrosis and multinucleated giant cells [9].
Hansen disease has a variable presentation depending on the spectrum ranging from the tuberculoid to the lepromatous pole. Peripheral nerves are involved. Erythematous plaques are usually present in the TT, BT, and BB types. Histopathology shows epitheloid granulomas involving the grenz zone; infiltrate is present around the dermal nerves. In some cases one can demonstrate AFB.
Cutaneous Leishmaniasis begins as a papule at the site of inoculation and progresses to ulcerated nodules and plaques. Most forms heal spontaneously. Tissue smears demonstrating LD bodies help in the diagnosis.
Pseudolymphoma is a benign but persistent lymphoid proliferation in the dermis and can be related to a wide spectrum of benign diseases such as hypersensitivity reactions and premycotic conditions. Histologically, there is proliferation of the epidermis with changes of spongiosis, vascular proliferation. The lymphocytic infiltrate is pronounced in upper dermis [10].
Granuloma faciale is a rare dermatosis of uncertain etiology clinically presenting as nodules and plaques. This condition mainly involves the face without any systemic involvement and it is histologically characterized by a polymorphous infiltrate with evidence of leucocytoclastic vasculitis [11].
Discoid lupus erythematosus is an autoimmune disorder affecting women in preference to men, mainly in the child bearing ages. The lesions involve the face in 85 percent of cases. Clinically, it is characterized by well demarcated, edematous, scaly papules and plaques that exhibit hypopigmentation and scar on resolution. Histologically, an interface changes are prominent features.
Conclustion
All the diseases mentioned in the discussion should be kept in mind when one sees this type of plaque-like presentation. Histological similarities make it further difficult to differentiate granulomatous rosacea from its mimickers. The diagnosis can be arrived at by meticulous history, clinical examination, laboratory and imaging, and clinical-pathological correlation, which is vital in view of the striking differences in the management of these conditions.
Our patient with granulomatous rosacea and mid face edema did not respond well to oral tetracycline, but resolved with a combination of isotretinoin for 6½ months and prednisolone tapered over about 8 weeks.
References
1. Cohen AF, Tiemstra JD. Diagnosis and treatment of rosacea. J Am Board Fam Pract. 2002;15:214-7. [PubMed]2. Helm KF, Menz J, Gibson LE, et al. A clinical and histopathologic study of granulomatous rosacea. J Am Acad Dermatol 1991;25:1038-43. [PubMed]
3. Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol 2002;46:584-7. [PubMed]
4. Mullanax MG, Kierland RR. Granulomatous rosacea Arch Dermatol 1970; 101:206-211. [PubMed]
5. Patrinely JR, Font RL. Anderson RL. Granulomatous acne rosacea of the eyelids. Arch Ophthalmol 1990; 108:561-563. [PubMed]
6. Helm KF, Menz J, Gibson LE, A clinical and histopathologic study of granulomatous rosacea. J Am Acad Dermatol 1991; 25:1038-1043. [PubMed]
7. Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008. 33(6):764-7. [PubMed]
8. Gawkrodger DJ. Sarcoidosis. In: Burns T, Breathnach S, Cox N, Griffith C, editors. Rook’s Textbook of dermatology. 7th ed. London: Blackwell sciences; 2004. P.1-58.
9. Handa S, Bambry P. Sarcoidosis and other Granulomas. In: R.G. Valia, Ameet R. Valia, editors. IADVL Textbook of Dermatology. 3rd ed. Mumbai: Bhalani publishers; 2008. P. 1343.
10. Brodell RT, Santacruz DJ. Cutaneous pseudolymphoma. Dermatology clin. 1985; 4:719-734. [PubMed]
11. Burgdorf WHC. Granuloma faciale. In: Freedberg IM, Eisen AZ, Wolf K, et al, editors. Fitzpatrick’s Dermatology in general medicine. 6th ed. New York: McGraw-Hill; 2003. P. 967-69.
© 2011 Dermatology Online Journal

