Folliculotropic mycosis fungoides and a leonine clinical appearance of the face
Published Web Location
https://doi.org/10.5070/D30w86n2qxMain Content
Folliculotropic mycosis fungoides and a leonine clinical appearance of the face
Tomonobu Ito, Toshiyuki Yamamoto, Yuka Matsumoto, Junko Wakamatsu, Yukihiko Kato, Ryoji Tsuboi
Dermatology Online Journal 14 (9): 6
Department of Dermatology, Tokyo Medical University, Tokyo, Japan. itoto@niaid.nih.gov Abstract
A 73-year-old man presented with a two year history of multiple nodules and follicular papules accompanied by slight itching on the face and the forearm. A physical examination showed multiple, soft, erythematous nodules on the forehead, cheek, and jaw, contributing to a generally leonine appearance of the face. Histopathological examination from the forehead revealed dense, massive concentrations of atypical lymphocytes in the dermis, and the forearm showed infiltration of atypical lymphocytes predominantly around the follicles. We diagnosed this condition as folliculotropic cutaneous T cell lymphoma (CTCL). EPOCH therapy was very effective and the lesions of the forehead and forearm showed a decrease in tumor elevation; the histology showed a precipitous decrease in the number of the atypical lymphocytes.
Mycosis fungoides (MF) is the most common type of cutaneous T cell lymphoma, characterized by an indolent clinical course with the subsequent evolution of patches, plaques, and tumors. Some variants and subtypes of CTCL, however, display uncommon clinical as well as histological features, and are often defined as folliculotropic, pagetoid, granulomatous, or 'slack skin' [1, 2]. We report a case of folliculotropic CTCL presenting a rare, leonine clinical appearance of the face.
Clinical synopsis
 |
| Figure 1 |
|---|
| Figure 1a. Multiple, soft, erythematous nodules on the forehead, cheek and jaw Figure 1b. Follicular papules were seen on the right forearm |
A 73-year-old man was referred to our department with a two year history of multiple nodules and follicular papules accompanied by slight itching on the face and the forearm. Six months prior to consultation, the nodules on his face began to increase rapidly in size. Physical examination showed multiple, soft, erythematous nodules, about 2cm in diameter on the forehead, cheek and jaw (Fig. 1a). Follicular papules were not seen on other regions besides the right forearm (Fig. 1b). The lymph nodes of the neck and axillae were not palpable. The peripheral white blood cell count, red blood cell count, and platelet count were within the normal range; atypical lymphocytes were not observed. The soluble interleukin (IL) - 2 receptor levels were within the normal range (445 U/mL; normal 167 - 497 U/mL). Computerized tomography and gallium scintigraphy (Ga67-SPECT) failed to reveal inflammatory lesions, tumors, or lymphadenopathy. No atypical cells were observed in the bone marrow.
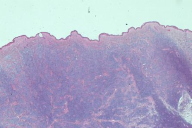
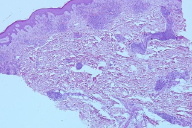
A skin biopsy taken from the forehead revealed dense, massive concentrations of atypical lymphocytes in the dermis (Figs. 2a & 2b). Histopathological examination of the forearm showed infiltration of atypical lymphocytes predominantly around the follicles (Fig. 3). There was no detectable involvement of the epidermis, and alcian blue stain failed to show mucinosis. Immunohistochemical analysis revealed that the majority of atypical lymphocytes were CD3+, CD4+ and CD8- T cells. A small number of CD30+ cells were present but no CD56+ cells were detected. Southern blot analysis of a skin specimen detected a monoclonal rearrangement of the T cell receptor β− chain gene and γ− chain gene.
THP-COP therapy with a regimen of pirarubicin hydrocholoride 30mg/m² day 1, cyclophosphamide 500 mg/m² day 1, vincristine 1 mg/m² day 1, and prednisolone 30 mg/m² day 1-5, was given without effect. EPOCH therapy (doxorubicine 10mg/m² for day 1-4, vincristine 0.4mg/m² for day 1-4, etoposide 50 mg/m² for day 1-4, cyclophosphamide 750 mg/m² for day 6, prednisolone 60 mg/body for day 1-6) was therefore begun. After 5 courses of EPOCH therapy, the lesions of the forehead and forearm showed a decrease in tumor elevation and the histology from a repeat biopsy showed a precipitous decrease in the number of atypical lymphocytes; the infiltrated atypical lymphocytes remained only around the follicles. The response was good, but not complete. The patient was then maintained with oral chemotherapy (etoposide 50 mg/day for 21 days per month) and prednisolone 10 mg/day without relapse for 24 months.
Discussion
Mycosis fungoides may evolve into tumor stage after protracted growth, but in the present case the lesions developed into a leonine clinical appearance within a relatively short period. According to previous literature, clinical leonine appearance of the face sometimes occurs in T cell lymphoma [3], photosensitivity [4], sarcoidosis [5], and leprosy. In the present case, however, there was no mucinosis, photosensitivity, nor infection.
According to the studies of the Dutch Cutaneous Lymphoma Group, the clinical features 51 patients diagnosed with folliculotropic MF were variable [6]. The most common type of skin lesion consisted of patches, plaques and papules, in addition to the usual nodules, tumors, and comedones. Among the reported cases of folliculotropic MF, the leonine appearance of the face was reported in two cases [7]. In general, the characteristic histopathological findings of folliculotropic MF include the primarily perivascular and periadnexal localization of the dermal infiltrates with variable infiltration of the follicular epithelium by small, medium-sized, or sometimes large hyperchromatic cells with cerebriform nuclei; sparing of the epidermis is usual. A biopsy specimen from the affected skin of the forehead in our case showed diffuse cellular infiltrations in the dermis, including adnexal structures, whereas the forearm showed infiltration of atypical lymphocytes only around the follicular epithelium. A second biopsy from the forehead after chemotherapy revealed tumor cell infiltration predominately around the hair follicles. In our case, follicular papules of the right forearm became the most important clue to the diagnosis.
There is no therapy that is considered the treatment of choice for folliculotropic MF. However, topical corticosteroids, PUVA, retinoids, nitrogen mustard, interferon-alpha, and electron beam therapies have been reported as being effective against folliculotropic MF [8, 9]. In the present case, the facial lesions consisted of multiple tumors that were unresponsive to PUVA and interferon therapy. Because our patient refused electron beam therapy, we used THP-COP therapy and then EPOCH therapy for five courses. Although complete remission was not achieved, we consider that EPOCH, a regimen for refractory cutaneous T-cell lymphoma, is an effective treatment for folliculotropic MF [9, 10]. Tumor stage folliculotropic MF has been reported to have a poorer prognosis than classical MF (tumor stage) [7]; long term careful follow up is essential.
References
1. Rein W, Elaine S. J, Günter B Lorenzo C, Emilio B, et al. WHO-EORTC classification for cutaneous lymphomas: Blood, 2005; 105: 3768-3785. [PubMed]2. Slater. D. N. The new World Health Organization-European Organization for Research and Treatment of Cancer classification for cutaneous lymphomas: a practical marriage of two giants: Br J Dermatol, 2005; 153 874-880. [PubMed]
3. Burg G, Dummer R, Kerl H. Classification of cutaneous lymphomas: Dermatol Clin, 1994; 12: 213- 217. [PubMed]
4. Volden G, Thune PR. Light sensitivity in mycosis fungoides: Br J Dermatol, 1977; 97: 279- 284. [PubMed]
5. Kendric CG, Brown RA, Reina R. Cutaneous sarcoidosis presenting as leonine facies: Cutis, 2004; 73: 57- 61. [PubMed]
6. Van Doorn R, Scheffer E, Willemze R. Follicular mycosis fungoides, a distinct disease entity with or without associated follicular mucinosis: a clinicopathologic and follow-up study of 51 patients: Arch Dermatol, 2002; 138: 191-198. [PubMed]
7. Vergier B, Beylot-Barrt M, Beylot C, de Mascarel A, Delaunay M et al. Pilotropic cutaneous T-cell lymphoma with out mucinosis: a variant of mycosis fungoides?: Arch Dermatol, 1996; 132: 683-687. [PubMed]
8. Requena L, Sanchez M, CoCa S, Sanchez Yus E. Follicular lymphomatoid papulosis. Am J Dermatopathol, 1990; 12: 67-75. [PubMed]
9. Akpek G, Koh HK, Bogen S, O'Hara C, Foss FM. Chemotherapy with etoposide, vincristine, doxorubicin, bolus cyclophosphamide, and oral prednisone in patients with refractory cutaneous T-cell lymphoma. Cancer, 1999; 86: 1368-1376. [PubMed]
10. Joseph MC, Eric DH, Francine MS. Lymphoma of the skin. Hematology Am Soc Hematol Educ Program, 2002; 263-82. [PubMed]
© 2008 Dermatology Online Journal