Cryotherapy for anogenital warts: factors affecting therapeutic response
Published Web Location
https://doi.org/10.5070/D30st3s692Main Content
Cryotherapy for anogenital warts: factors affecting therapeutic response
Abbas Rasi1, Razieh Soltani-Arabshahi1, Alireza Khatami2
Dermatology Online Journal 13 (4): 2
1. Department of Dermatology, Hazrat-e-Rasool University Hospital, Iran University Of Medical Sciences. r_arabshahi@yahoo.com2. Center for Research and Training in Skin Diseases and Leprosy, Tehran University of Medical Sciences, Tehran, Iran
Abstract
Human papilloma virus genital infection remains a treatment dilemma; there is still no gold standard therapy, treatment options are limited, expensive and often ineffective, and recurrence rates are relatively high. The primary objective of this study is to establish the efficacy, safety, and tolerability of cryotherapy in the treatment of these lesions. From 1999 to 2003, 100 consecutive patients with at least ten genital warts were treated with liquid nitrogen cryotherapy using a cotton-tipped applicator and two freeze-thaw cycles at the outpatient dermatology clinic of Hazrat-e Rasool University Hospital. Treatment was repeated every 3 weeks until the disappearance of all visible lesions was achieved. Patients were followed up every 4 months for 18 months. Complete clinical cure (CCC) was defined as complete clearance of all lesions and no evidence of disease for a minimum of 18 months. The CCC and relapse rate were evaluated based on different demographic and clinical characteristics. Overall, 86 percent of the patients achieved CCC after an average of 3.31 treatment sessions. All of the failed cases were attributed to recurrence of warts in new sites. The cure rate increased in parallel with increasing treatment sessions until the 6th session, after which it remained constant. The cure rate was lower and the number of treatment sessions higher in older patients. The age of the patient and number of treatment sessions affect the cure rate. The recurrence rate was significantly higher for the married or multi-partner group than for unmarried patients. We concluded that cryotherapy is an effective method for treatment of anogenital warts. The age of the patient and size of the lesions affect the cure rate. However, the most important factor in relapse of the lesions is unprotected sexual contact during and after treatment.
Introduction
External genital warts (EGWs) associated with human papillomavirus infection involve the external genitalia (i.e., penis, scrotum, vulvae), pubic area, perineal regions, and crural folds [1]. They manifest either as small papules (small, smooth, and dome shaped) or as large acuminate papules and plaques. HPV genital infection is considered to be the most prevalent sexually transmitted disease in the US and Europe, affecting 1-2 percent of the sexually active population between 15 and 49 years of age [2]. EGWs are difficult to treat because the virus produces small amounts of HPV antigen (located in relatively inaccessible areas of the epidermis) that can elude the immune system. In addition, after destructive treatments HPV DNA continues to reside in the margins outside of the treatment area [3].
The proper approach to the management of warts depends on the age of the patient, location, size, extent, and type of wart, and duration of lesions. The patient's immunologic status, cooperation, ability to pay, and tolerance of adverse reactions are also important factors that influence results [4, 5]. The ideal therapy should be effective (i.e., high clearance and low recurrence rates) and cause minimal local and systemic adverse effects. Different treatment options include various topical therapies (salicylic acid, cantharidin, podophyllin, podophylotoxin, 5-fluorouracil, or bleomycin), newer immunomodulatory treatments (imiquimod or interferons), and physical destruction (surgical excision, cryosurgery, electrodesiccation, or laser therapy).
The use of cold or freezing modalities have been important adjuncts in medicine since the Egyptians used these to treat injuries and inflammation around 2500 B.C.E. [6]. Allington used liquid nitrogen as a cryogen in 1948 [7]. Nowadays, cryotherapy with liquid nitrogen, applied with a cotton-tipped swab (or cryogun) to freeze visible warts along with halo of surrounding tissue is a common and effective treatment for most warts [8, 9]. Application of the cryogen induces skin and vascular damage, leading to both epidermal and dermal cellular necrosis. Usually, two freeze/thaw cycles are undertaken, but the optimal number of applications has not been established. Cryogenic agents are relatively inexpensive and easy to apply, usually require no anesthesia, and cause little scarring after re-epithelialization. The treatment does not have systemic or distant cutaneous side effects. Pigmentary changes are not uncommon but are usually short term.
Genital wart clearance rates of 79-88 percent are reported with cryotherapy alone or together with adjuvant treatments. However, 25-39 percent of cases experience recurrences despite multiple treatments [10, 11]. The purpose of this study was to evaluate the clinical response of anogenital warts to cryotherapy with liquid nitrogen and explore the causes of relapse.
Patients and methods
Patients with anogenital warts seen consecutively in the outpatient dermatology clinic, Hazrat-e Rasool University Hospital, Tehran, Iran, from 1999 to 2003, were enrolled in the study after obtaining written informed consent. The diagnosis was based on the clinical appearance of the lesions. Patients were eligible for the study if they had at least 10 easily identifiable warts on the genital area and had not received any therapy for genital warts for at least 6 months. Patients who had a history of keloid or cold sensitivity were excluded from the study. All patients underwent serologic testing for Hepatitis B surface antigen, Hepatitis C antibody, VDRL, and HIV antibody.
Clinical and demographic characteristics of all patients, including age at diagnosis, sex, type and location of lesions, frequency of recurrences, and history of sexual contacts were recorded in a predesigned proforma. Photographs were obtained at the beginning of the study. Genital warts were categorized as (i) small papular lesions less than 0.7 mm in diameter, with a smooth surface or (ii) large condyloma acuminatae more than 0.7 mm in diameter, with an irregular surface, often with finger-like projections.
The study was approved by human studies subcommittee of the University.
Technique
All eligible patients were treated with liquid nitrogen cryotherapy. Liquid nitrogen was poured from the vacuum flask into a small stainless steel cup for each patient. A loosely wrapped cotton-tipped applicator shaped slightly smaller than the lesion was dipped into the nitrogen and promptly placed onto the cutaneous lesions. Thick, hyperkeratotic lesions were treated by applying moderate pressure and rolling the applicator over the surface of lesions, without prior de-bulking. Small lesions were identified with the help of a hand lens and were treated by frequently interrupting contact between the applicator and skin, thus preventing the zone of freezing from extending to a greater depth and width than necessary. At each visit, we treated all the visible lesions at one sitting.
Liquid nitrogen was applied repeatedly until the white freezing front extended 1-3 mm onto the surrounding normal skin. For each lesion, two cycles of a full freeze (5-30 seconds for smaller lesions on scrotum or penile shaft and 30-60 seconds for larger lesions) and a thaw of at least 60 seconds were performed. No dressing was required. In cases that developed large or hemorrhagic blisters, we tried to decompress the affected lesion with a sterile surgical blade or needle, leaving the roof intact. Treatment was repeated every 3 weeks until total clearance of the lesions. The number of treatment sessions was dictated by clinical response of the patients.
Because the lesions were mostly small in diameter, even though numerous, patients generally tolerated cryotherapy well without requiring topical anesthesia. No analgesics other than aspirin or acetaminophen were required.
Follow-Up
Patients received no treatment for the warts other than cryotherapy throughout the study. Clinical evaluation was performed by the treating physician as well as another dermatologist, at baseline and at each clinical visit every 3 weeks until complete clinical response. Thereafter, patients were reviewed at 4-month intervals for a further 18 months. Clinical response and adverse sequelae (hyperpigmentation, hypopigmentation, and scar formation) were assessed at the target wart site and in the surrounding area. At each follow-up visit, advice regarding sexual contact avoidance was reinforced.
Complete clinical cure (CCC) was defined as complete clearance of all genital warts with no evidence of disease (recurrence at the same site or reoccurrence at another site). Any patient, who was clinically cured but had a recurrence or reoccurrence during the follow-up period, was considered a treatment failure.
Statistical Analysis
Data were transferred to SPSS version 13.5. The Pearson, chi-Square, and Fisher's exact test were used for statistical analysis and p < 0.05 was accepted as significant.
Results
A total of 100 patients with genital warts (93 males, 7 females, mean age at diagnosis 31.72± 7.89, range 18-56) were treated with liquid nitrogen cryotherapy. The duration of genital warts before treatment was from 8 to 40 months. Lesions ranged from 0.2 x 0.2 to 1.0 x 1.5 cm. None of the patients had positive serology for HIV, hepatitis B, hepatitis C, or a positive VDRL.
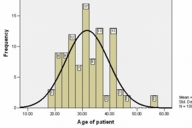
Three age groups were analyzed: 0-19 years (3%); 20-39 (77%); and 40-59 (20%). Figure 1 shows the age distribution of the patients. We did not find any statistically significant association between frequency of genital warts and age of the patients.
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Age of patients with genital warts at diagnosis Figure 2. Anatomic locations of genital warts | |
Figure 2 shows the anatomic distribution of genital warts in the study patients. The pubis (72.0 %) or penile shaft (69.9 %) was affected in all of the male patients. The involvement of the scrotal area was less frequent (2.2 %) and always accompanied by pubic or penile lesions. We did not find perianal lesions in any of the male patients. In all of the seven female patients, the pubis and perianal area were involved. Sites of involvement were significantly different between female and male patients (chi2 test, p < 0.001). Extragenital warts were not found in any of the patients.
Small papular lesions were present on 74 patients. Large condylomas were present on 26 patients. Large condylomas were identified in 65 percent of patients over age 40, 16.9 percent of patients 20-39 years old, and none of the patients under 20; the difference was statistically significant (chi square, p < 0.001).
Of the 100 patients, 43 were unmarried but without a regular sexual partner (UM), 24 were unmarried and had multiple partners (MP), and 33 were married (MA). The MA and MP groups had similar baseline demographic (sex and age) characteristics as well as regular sexual contacts, so we put them in one common group, MAP.
Overall, 86 of 100 patients (86 %) achieved CCC after an average of 3.31 treatment sessions. Considering all patients, 58 percent achieved CCC within 3 sessions and 28 percent needed 4-6 sessions for CCC. The cure rate did not increase further by increasing the number of treatment sessions to more than 6. None of the patients who achieved CCC experienced relapse in the 18 month followup period. Fourteen cases did not achieve complete clinical cure because of continued development of new lesions. All of these failed cases were from development of EGWs in another site; no cases of recurrent lesions in the same site were seen after successful treatment. In patients who developed new lesions in spite of using condoms, all of the new lesions involved non-protected sites of the genital area.
Age was a significant variable affecting outcome. Cure rate was 100 percent in patients under age 20, 90.9 percent in patients aged 20-39, and 65 percent in patients over age 40. The difference was statistically significant (chi square, p = 0.009). Furthermore, the number of treatment sessions to achieve CCC was less in younger patients (p = 0.004). Most (68.8 3%) of the patients under age 40 needed 2-3 treatment sessions, whereas 75 percent of patients over 40 needed more than 3 treatment sessions. Reoccurrence rate was also significantly higher in older patients (p = 0.009), with the greatest rate of recurrences (35 %) seen in patients over age 40.
The response rate was higher in small warts than large condylomas but the difference was not statistically significant (86.5 % versus 84.6%, p = 0.813). We did not find any significant correlation between the size of the wart and the number of treatment sessions.
Marital state and sexual contacts were significant factors affecting outcome. All of the unmarried patients who did not have regular sexual contacts achieved CCC; whereas, 18.2 percent of the married (single partner) and 33.3 percnet of the multi-partner patients experienced relapse. Overall, reoccurrence rate was significantly higher in the MAP group than in the UM patients (24.6 % vs. 0 %, p < 0.001). The number of treatment sessions was also significantly different between UM and MAP groups (chi square, p < 0.001). All of the UM individuals (100 %) achieved CCC within 3 sessions; 26.3 percent of the MAP group patients achieved CCC in 3 sessions and 49.1 percent of them needed 4-6 sessions.
In all patients, excellent tissue preservation was achieved and no instances of cold sensitivity, infection, ulcers, alopecia, nerve damage, scarring, or keloid formation were reported. The average healing time was 5-7 days. Treatment-related adverse events were confined to the application site and included hyper- and hypo-pigmentation in 17 percent and 16 percent of the patients, respectively. Both hyperpigmentation and hypopigmentation were more common after treatment of large lesions (chi square, p = 0.005 and 0.001). Hyperpigmentation was slightly more frequent in patients who received at least 6 treatment sessions than in patients with fewer than 3 treatment sessions, but the difference was not statistically significant (21 % vs. 17.2 %, p = 0.842). Hypopigmentation occurred in 13.8 percent of patients who were teated for fewer than 3 sessions and 21.4 percent of those who received more than 6 sessions. Again, the difference did not reach statistical significance (p = 0.745). Adverse effects did not warrant suspension or discontinuation of therapy in any of the patients.
Discussion
Cryotherapy uses freezing temperatures to destroy tissue via intracellular and extracellular ice crystal formation, disruption of cell membranes, and circulatory changes in the skin [12]. In a controlled study by Damstra and Van Vloten [13], a fine needle-spray technique was used to treat 64 patients with small penile and vulvar condylomas; a 92 percent remission rate was achieved after 3 months. In other therapeutic trials using cryotherapy for EGWs, clearance rates of 54-88 percent and recurrence rates of 21-40 percent are reported [14, 15, 16, 17]. In most cases, liquid nitrogen had better clearance rates than TCA or podophyllin, but it may be less effective than surgical excision and electrodesiccation [18].
Our results show an 86 percent clearance rate within a maximum of 6 treatment sessions. None of our cured patients had a relapse during the follow-up period. This result is much better than the 25-67 percent recurrence rate in previous studies [11]. The use of a good hand magnifier, inspection of lesions under good light, and treatment of all suspicious lesions at each time were factors in improving therapeutic outcome. Some investigators believe that recurrences are often at sites of previous genital warts, attributed to the reactivation of virus at the site of previous clearance [19]. However, if the tissues containing the wart virus are completely destroyed (complete clinical cure), there may be much less risk of recurrence of the lesions in the same sites. The high recurrence rate reported in different studies might be from development of new lesions in previously unaffected sites because of re-exposure to the infection or from reactivation of quiescent virus. Fourteen percent of our patients did not respond to cryotherapy (failed cases) and experienced continued development of warts in different sites. Theoretically, failure in clinical response could result from low efficacy of the chosen method of therapy, intrinsic refractoriness of the lesions, hidden intragenital lesions in their partners or reactivation of viruses from adjacent normal appearing skin.
In order to investigate factors leading to treatment failure, we further analyzed treated and failed cases. Neither sex nor site of the lesion had any significant impact on relapse or reoccurrence of warts. However, sex was a significant factor in determining the site of involvement. Difference in the involved sites (particularly frequency of perianal lesions) between males and females reflects different sexual practices in men and women. Perianal and intra-anal warts are present primarily in patients who have had receptive anal intercourse. However, these warts can occur in patients without any history of anal intercourse [10]. In this study, scarcity of perianal verrucae in men might point to the low level of anal intercourse in our male patient population.
Infection with high-risk types of HPV and older age are assumed to be risk factors for persistence of genital warts [19]. In our study, the highest response rate and lowest number of treatment sessions were seen in patients younger than age 20, whereas patients over 40 showed the worst clinical outcome. However, the most important difference between treated and failed cases was sexual activity. Clinical cure occurred more rapidly with fewer treatment sessions in the UM group. A relapse rate of zero in unmarried patients who did not have regular sexual contacts is impressive when compared to 24.6% in the MAP group who had single or multiple regular sexual contacts. This highlights a benefit of sexual abstinence in ensuring complete clinical cure and minimizing relapse of the lesions. With regard to the above findings, we hypothesize that the major source of recurrence is continued sexual contact with an infected partner. This risk, irrespective of age, is particularly related to marital state and number of sexual contacts. Thus, the best way to ensure complete clinical cure would be detailed physical exam and treatment of verrucae in both partners, together with sexual abstinence until resolution of all of the lesions. All of the failed cases were attributed to lesions in new sites, not recurrence of the old lesions in the treated site. Because of the significant influence of sexual partners on the outcome, we conclude that in our patients the quiescent virus in the apparently normal looking skin of the patients with genital warts did not have a major role in recurrence and/or recurrence of the lesions.
Following the mentioned treatment protocol, the overall adverse effects were subtle and mostly seen after treatment of large lesions. The most frequent adverse effect was temporary hyperpigmentation in 17 percent of patients; this disappeared within 9 months with regular use of topical steroids, glycolic acid, retinoids, and hydroquinones. In fact, maintenance of a normal dermal fibrous network after freezing, allows the lesions to heal without scarring [8, 11].
Conclusion
In conclusion, this study supports the previous observations that cryotherapy with liquid nitrogen is an effective, simple, safe, and well tolerated treatment option for localized as well as multiple anogenital warts. Our aggressive cryotherapy treatment regimen was associated with a low recurrence or reoccurrence rate. Our data suggest that a permanent cure is possible. However, persistence of verrucae in the sexual partner(s) of the patient might cause reoccurrence of new warts.
Acknowlgment: The authors would like to thank Dr Maryam Hoseinnejad for statistical analysis.
References
1. Centers for disease control (CDC). Sexually transmitted diseases treatment guidelines. MMWR Morb Mortal Wkly Rep. 1989 Sep;38(suppl.8):18-21. PubMed2. Koutsky LA, Galloway DA, Holmes KK. Epidemiology of genital human papillomavirus infection. Epidemiol Rev1988;10:122-63. PubMed
3. Coleman N, Birley HD, Renton AM, Hanna NF, Ryait BK, Byrne M, Taylor-Robinson D, Stanley MA. Immunological events in regressing genital warts. Am J Clin Pathol. 1994 Dec;102(6):768-74. PubMed
4. Beutner KR, Ferenczy A. Therapeutic approach to genital warts. Am J Med. 1997 May;102(5A):28-37. PubMed
5. Sterling JC, Handfield-Jones S, Hudson PM; British Association of Dermatologists. Guidelines for the management of cutaneous warts. Br J Dermatol. 2001 Jan;144(1):4-11. PubMed
6. Sguazzi A, Bracco D. A historical account of the technical means used in cryotherapy. Minerva Med. 1974 Oct;65(70):3718-22. PubMed
7. Allington HV. Liquid nitrogen in the treatment of skin diseases. Calif Med. 1950 Mar;72(3):153-5. PubMed
8. Ahmed I, Agarwal S, Ilchyshyn A, Charles-Holmes S, Berth-Jones J. Liquid nitrogen cryotherapy of common warts. Cryo-spray vs. cotton wool bud. Br J Dermatol. 2001 May;144(5):1006-9. PubMed
9. Kuflik EG. Cryosurgical treatment of periungual warts. J Dermatol Surg Oncol. 1984 Sep:10(9):673-6. PubMed
10. Kodner CM, Nasraty S. Management of genital warts. Am Fam Physician. 2004 Dec;70(12):2335-42. PubMed
11. Scheinfeld N, Lehman DS. An evidence-based review of medical and surgical treatments of genital warts. Dermatol Online J. 2006 Mar;12(3):5. PubMed
12. Connolly M, Bazmi K, O'Connell M, Lyons JF, Bourke JF. Cryotherapy of viral warts: A sustained 10-s freeze is more effective than the traditional method. Br J Dermatol. 2001 Oct;145(4):554-7. PubMed
13. Damstra RJ, van Vloten WA. Cryotherapy in the treatment of condylomata acuminata: a controlled study of 64 patients. J Dermtol Surg Oncol. 1991 Mar;17(3):273-6. PubMed
14. Handley JM, Horner T, Maw RD, Lawther H, Dinsmore WW. Subcutaneous interferon alpha 2a combined with cryotherapy vs cryotherapy alone in the treatment of primary anogenital warts: a randomised observer blind placebo controlled study. Genitourin Med. 1991 Aug;67(4):297-302. PubMed
15. Eron LJ, Alder MB, JM OR, Rittweger K, DePamphilis J, Pizzuti DJ. Recurrence of condylomata acuminata following cryotherapy is not prevented by systemically administered interferon. Genitourin Med. 1993 Apr;69(2):91-3. PubMed
16. Abdullah AN, Walzman M, Wade A. Treatment of external genital warts comparing cryotherapy (liquid nitrogen) and trichloroacetic acid. Sex Transm Dis. 1993 Nov-Dec;20(6):344-5. PubMed
17. Godley MJ, Bradbeer CS, Gellan M, Thin RN. Cryotherapy compared with trichloroacetic acid in treating genital warts. Genitourin Med. 1987 Dec;63(6):390-2. PubMed
18. Wiley DJ. Genital warts. Clin Evid. 2002 Dec;(8):1620-32. PubMed
19. Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med. 1998 Feb;338(7):423-8. PubMed
© 2007 Dermatology Online Journal

