Primary cutaneous actinomycosis caused by as first manifestation of HIV infection
Published Web Location
https://doi.org/10.5070/D30n05580mMain Content
Primary cutaneous actinomycosis caused by Actinomyces meyeri as first manifestation of HIV infection
J Gomes1, T Pereira1, A Carvalho2, C Brito1
Dermatology Online Journal 17 (11): 5
1. Department of Dermatology and Venereology, Hospital de Braga, Portugal2. Department of Internal Medicine, Hospital de Braga, Portugal
Abstract
Primary cutaneous actinomycosis is very uncommon. We report a patient with cutaneous actinomycosis with multiple lesions without any detectable extra-cutaneous lesions. In our patient the actinomycosis was the presenting manifestation of HIV infection.
Introduction
Actinomyces are a group of filamentous bacteria belonging to the class Actinobacteria. In the past, microorganisms under this classification were wrongly classified as fungi because of their tendency to produce branching filaments.
Most of the pathogenic actinomycetes occur in nature and belong to the soil saprophytic flora. Pathogenic anaerobic actinomycetes are normal inhabitants of the human mouth, respiratory, intestinal, and genito-urinary flora. Usually, actinomycosis is therefore acquired endogenously [1, 2, 3, 4].
Described by Israel in 1878, the disease has a worldwide distribution. Since the introduction of antibiotics, there is a tendency to miss subtle cases with more limited involvement, many of them limited to the oral cavity. Species known to cause disease in humans include A. israelii, and less often, A. naeslundii, A. gerencseriae, A. viscosus, A. odontolyticus, and A. meyri [2]. Actinomycosis can affect all organs and tissues of the body. Five main clinical types can be recognized, depending on the primary site of infection. These are cervicofacial, thoracic, abdominal, primary cutaneous, and pelvic presentations [1]. Cervical actinomycosis is the most frequent form of disease, accounting for approximately 55 percent of cases. Primary cutaneous actinomycosis is very uncommon and usually occurs on the exposed skin [1].
Case report
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Necrotic ulceration surrounded by an erythematous halo. Figure 2. Lesion at the right thigh with ulceration and indurated borders | |
We report a case of a 23-year-old man hospitalized for fever and weight loss, who presented with a two-month history of painful, ulcerated skin lesions draining purulent material. The lesions had started on the right axilla in a localized area, then spread to the trunk and the upper and lower extremities. He exhibited erythematous nodules, which ulcerated and discharged seropurulent material (Figures 1 and 2). He also reported fever, with nocturnal sweating and weight loss (7 Kg in two months). There were no others abnormalities in his physical examination.
The patient was previously treated with oral ciprofloxacin (500 mg/bid) without improvement.
 |
| Figure 3 |
|---|
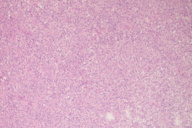
| Figure 3. Abundant neutrophilic inflammatory infiltrate with multinucleated cells. |
Skin biopsy from a lesion showed an abundant dermal and subcutaneous neutrophilic inflammatory infiltrate, with areas of suppuration and granuloma formation (Figure 3). Culture of biopsy fragments produced colonies of Actinomyces meyeri.
Laboratory studies disclosed a mild pancytopenia, with a WBC of 3.6 x 10³/μl, hemoglobin of 11.9 g/dL, platelet count 118 x 10³/μl, CD4 cell count of 123/μl, HIV 1 positive with viral load of 183404 copies/ml.
Other investigations, such as chest X-ray, abdominal and pelvis ultrasonography, and urine and blood cultures were normal or negative.
 |  |
| Figure 4 | Figure 5 |
|---|---|
| Figure 4. Lesions after 4 months of treatment. Figure 5. Atrophic scar after treatment | |
A diagnosis of primary cutaneous actimomycosis in a patient with HIV infection was made. We performed wound debridement and the patient was treated with trimethoprim 160 mg in combination with sulfamethoxazole 800 mg (TMP+SMX) twice a day orally. Anti-retroviral therapy (ART) with emtricitabina + tenofovir, ritonavir, and darunavir was initiated.
After 4 months of this therapy almost all lesions had healed with atrophic scars (Figures 4 and 5).
Discussion
Actinomycosis is an uncommon infectious disease, characteristically chronic, with spreading suppurative and granulomatous lesions [1, 2, 3, 5]. The primary cutaneous form is very rare [3, 5, 6]. Usually, there is a significant delay between the initial appearance of the skin lesions and the subsequent diagnosis [2].
Here we report a patient with cutaneous actinomycosis with multiple lesions without any detectable extra-cutaneous lesions. There were no cervicofacial, thoracic, or abdominal lesions. These findings suggest that cutaneous disseminated actinomycosis in our patient developed primarily in the skin. Although the patient did not recall any trauma, we presumed the infection was linked to minor trauma, because the patient lived in a rural region. Post-traumatic actinomycosis and cases caused by insect or human bites have been described previously. In our case A. meyeri was isolated, which is an oral saprophytic obligate anaerobe. It differs from other Actinomyces organisms by morphological and biochemical features and by a great propensity to disseminate [4, 7].
In our patient the actinomycosis was the presenting manifestation of HIV infection, already at AIDS stage.
Cutaneous disorders occur in nearly every patient during the course of HIV disease. The spectrum of dermatologic manifestations is very broad and diverse. Identification of HIV-associated dermatologic disease may therefore lead to testing and diagnosis.
The treatment of actinomycosis requires high-dose antibiotics to be given for a long period. A good rule is to continue therapy until full resolution of all clinically evident disease. Generally the treatment of choice is penicillin, but actinomyces spp. are sensitive to several antibiotics that are effective against Gram-positive organisms, such as penicillin, sulfonamides, streptomycin, tetracyclines, erythromycin, and rifampicin. In severe cases the antibiotics should be administered intravenously for several weeks, followed by wide surgical excision of the remaining infected tissue. If there is marked fibrosis in the lesions, effective drug levels are difficult to achieve. These recommendations were developed at a time when patients with actinomycosis typically presented late in the course of the disease. However, our patient had multiple lesions, restricted to the skin, that were recent and there was minimal fibrosis. He started an oral combination of TMP+SMX and ART. Although the patient was immunocompromised he improved notably on this regimen. We believe that this was also related to a response to ART with an increase in CD4+ counts to >200 cells/μL. There are other cases of success with TMP+SMX in the literature, although its use is controversial.
This case is of particular interest because of the extracervical localization with disseminated lesions, the rare species isolated, and the fact that it was the first manifestation of immunossupression in a patient with unknown HIV infection.
References
1. Romano C, Massai L, De Aloe GB, Schurfeld K, Miracco C. A case of primary cutaneous actinomycosis. Acta Derm Venereol. 2002;82(2):144-5. [PubMed]2. Brion N, Bertail MA, Denis C, Auffret N, Civatte J. Disseminated actinomycosis presenting with multiple subcutaneous abscesses. Ann Med Interne. 1981;132(5):328-32. [PubMed]
3. Mehta V, Balachandran C. Primary cutaneous actinomycosis on the chest wall. Dermatol Online J. 2008 Aug 15;14(8):13. [PubMed]
4. Liaudet L, Erard P, Kaeser P. Cutaneous and muscular abscesses secondary to Actinomyces meyeri pneumonia. Clin Infect Dis. 1996 Jan;22(1):185-6. [PubMed]
5. Verma KK, Lakhanpal S, Sirka CS, Khaitan BK, Ramam M, Banerjee U. Primary cutaneous actinomycosis. Acta Derm Venereol. 1999 Jul;79(4):327. [PubMed]
6. Roy D, Roy PG, Misra PK. An interesting case of primary cutaneous actinomycosis. Dermatol Online J. 2003 Dec;9(5):17. [PubMed]
7. Apothéloz C, Regamey C. Disseminated infection due to Actinomyces meyeri: case report and review. Clin Infect Dis. 1996 Apr;22(4):621-5. [PubMed]
© 2011 Dermatology Online Journal

