Atypical and unusual clinical manifestations of contact dermatitis to clothing (textile contact dermatitis) - case presentation and review of the literature
Published Web Location
https://doi.org/10.5070/D30kd1d259Main Content
Atypical and unusual clinical manifestations of contact dermatitis to clothing (textile contact dermatitis): Case presentation
and review of the literature
Aneta Lazarov MD1, Mario Cordoba MD2, Natalia Plosk MD3, David Abraham MD1
Dermatology Online Journal 9 (3): 1
1. Contact Dermatitis Clinic, Meir Hospital, Kfar Saba. 2. Department of Pathology, Meir Hospital, Kfar Saba, affiliated with
the Sackler School of Medicine, Tel Aviv University, Israel. 3. Dermatology Clinic, Herzeliya. lazarova@clalit.org.ilAbstract
Although the exact incidence of textile contact dermatitis is unknown, recent studies demonstrate that contact dermatitis produced by allergic or irritant reactions to clothing not only is more frequent than previously thought but also increasing. The clinical features of contact dermatitis (CD) caused by clothing may resemble common allergic contact dermatitis or may have atypical presentations. We report on several cases of clothing-induced contact dermatitis with atypical clinical presentations.
The exact incidence of textile contact dermatitis is unknown, but recent studies demonstrate that contact dermatitis produced by allergic or irritant reactions to clothing is more frequent than previously thought. [1, 2, 3, 4] It also has been shown that the frequency of textile-dye allergy is increasing.[5, 6]
The clinical features of contact dermatitis (CD) caused by clothing may resemble common allergic contact dermatitis or may have atypical presentations. The diagnosis of contact dermatitis caused by clothing may be difficult in some cases because of the wide spectrum of clinical presentations, including unusual clinical patterns and atypical localization. In this report, we discuss several cases of clothing-induced contact dermatitis that presented atypically.
Methods
All patients were patch tested with the standard series (TRUE Tests), textile color and finish series (TCFS), and clothing extracts. The TCFS was obtained from Chemotechnique Diagnostics (Malmo, Sweden) and included 32 allergens (13 disperse dyes, 8 reactive dyes, 3 acid dyes, 1 basic dye, 1 direct dye and 6 textile-formaldehyde resins). The allergens, applied on square chambers with micropore tape, were placed on unaffected skin of the upper back, removed at day 2 and read at days 2, 3, and 7, according to standard patch test procedure.[7] Some of the patients were patch tested with extracts of the suspected garments. The extract procedure was as follows: 2 cm of the cloth was immersed separately in 5 cc of water, ethanol 70 percent, and acetone for 30 minutes. The clothing was removed and the extracts with the water and alcoholic solutions were prepared for patch testing. Acetone extract (1 cc) was diluted with 3 cc of water, and this solution was used for patch testing. A 1 cm piece of clothing, having been immersed in water, was also applied, unaltered, for patch testing.
Case presentations
Erythema multiforme-like textile CD
Case 1.—A 44-year-old, atopic woman presented with a pruritic, widespread eruption on her abdomen and inner thighs, which disseminated to the lower back and upper extremities. The present eruption developed 1 week after the patient wore a new blue suit of synthetic material. A large area of erythema was seen on the patient's abdomen. This area was in direct contact with the trousers (Fig. 1). Erythematous macules and urticarial papules and plaques, some of them target-like, were observed on the inner thighs, shins, and upper extremities, in a manner resembling erythema multiforme (Fig. 2).
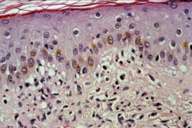
A lesional biopsy revealed mild focal spongiosis of the epidermis and a mild perivascular infiltrate composed of lymphocytes and eosinophils. The eosinophils were also conspicuous in the interstitial areas a (Figs. 3, 4). Patch testing results are shown in Table 1 and Figure 5. The erythema-multiforme-like eruption resolved within 14 days after exposure to the blue synthetic suit was discontinued.
In the past she had developed a similar eruption at and near the sites of metallic suture clips on her lower abdomen, after Caesarean section. Patch testing then demonstrated hypersensitivity (+2) to nickel sulfate. The metal clips were reported by the manufacturer as containing nickel. She was diagnosed as having erythema-multiforme-like CD related to nickel allergy.
 |  |
| Figure 1 | Figure 2 |
|---|
 |  |
| Figure 3 | Figure 4 |
|---|
 |  |
| Figure 5 | Figure 6 |
|---|
Case 2.—A 32-year-old healthy woman presented with an eruption of pruritic, erythematous macules and urticarial papules on her shins, resembling erythema multiforme lesions (Fig. 6). An allergic reaction to the beige synthetic stockings worn by the patient was suspected. Patch test results, as shown in Table 1, confirmed this relationship.
Purpuric textile CD
 |  |
| Figure 7 | Figure 8 |
|---|
Case 3.—A 64-year-old healthy man presented with purpuric papules and plaques affecting his lower extremities (Fig. 7) and arms. The lesions appeared in the winter, 1 month after he began wearing a dark blue synthetic sportswear while playing tennis.
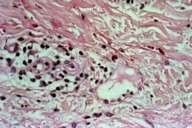
A lesional biopsy demonstrated spongiosis of the epidermis with areas of acanthosis. The inflammatory infiltrate was mainly perivascular and consisted of lymphocytes, eosinophils, and extravasated erythrocytes (Fig. 8). Some erythrocytes were observed in the epidermis.
Patch testing (Table 1) revealed a purpuric patch at the site of the tested allergen, Disperse Blue 124. A biopsy at this test site revealed spongiosis, exocytosis, and a perivascular, lymphocytic infiltrate. Extravasated erythrocytes were seen in the dermis and the epidermis. Complete involution, with no recurrence of the lesions, occurred 40 days after discontinuing the use of the blue suit and other darkly colored garments and provided further evidence for the etiological role of hypersensitivity to textile dyes in the development of this patient's purpuric dermatitis.
| Allergens | 1 EM | 2 EM | 3 Purpuric | 4 Papular | 5 Pigmented | 6 Pruritus | 7 Atopic |
|---|---|---|---|---|---|---|---|
| Nickel Sulfate | +2 | +1 | |||||
| Formaldehyde | +1 | +1 | |||||
| PPD | +1 | ||||||
| Mercapto mix | +1 | ||||||
| Quarternium 15 | +1 | ||||||
| Disperse Blue 106 | +1 | +1 | +1 | ||||
| Urea formaldehyde (Kaurit S) | +2 | +1 | |||||
| Melamine formaldehyde (Kaurit M 70) | +2 | +1 | |||||
| Disperse Blue 85 | +2 | +1 | |||||
| Disperse Blue 124 | +1 | +2 | +1 | +1 | |||
| Direct Orange 34 | +1 | ||||||
| Piece of suspected garment | +1 | +1 | +1 | +1 | |||
| Alcohol extract of garment | +1 | +1 | |||||
| Acetone extract of garment | +1 | +1 |
Papular and purpuric textile CD
 |  |
| Figure 9 | Figure 10 |
|---|
 |
| Figure 11 |
|---|
Case 4.—A 58-year-old man was evaluated because of a pruritic, papular rash that appeared 3 weeks after he started wearing new shirts bought in Turkey. Multiple, erythematous and livid papules were seen on his lower back and flanks. The lesions had a linear distribution at the waistband (Figs. 9, 10). Patch testing results are shown in Table 1 and Figure 11. Histopathological investigation of a papular lesion demonstrated spongiosis and acanthosis of the epidermis. A mixed inflammatory infiltrate consisting of lymphocytes, eosinophils, and multiple erythrocytes were seen both perivascularly and in the interstitial area. Similar clinical and histological findings were observed from a patch-test site positive for urea-formaldehyde. The lesions involuted completely and did not reappear after the patient stopped wearing the newly purchased shirts.
Pigmented textile CD
 |
| Figure 12 |
|---|
Case 5.—A 23-year-old healthy female presented with pruritic, hyperpigmented patches on her neck, chest (Fig. 12) and arms, which appeared some months after she began to wear synthetic, dark-colored, turtle-neck blouses. Examination revealed hyperpigmented patches at the same areas. Patch testing (Table 1) demonstrated a hypersensitivity reaction to Disperse Blue 106, Disperse Blue 124, a piece of a blouse, and an acetone extract of the garment. The lesions began to fade 1 year after exposure to dark synthetic garments was stopped.
Generalized pruritus with excoriation
 |  |
| Figure 13 | Figure 14 |
|---|
 |
| Figure 15 |
|---|
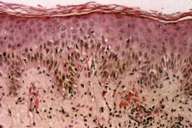
Case 6.—A 56-year-old, atopic woman presented because of severe generalized pruritus. Areas of excoriation could be seen on her trunk and extremities (Fig. 13, 14). A lesional biopsy demonstrated mild spongiosis and a mild perivascular lymphocytic infiltrate. Multiple eosinophils were seen in the perivascular and interstitial area. A diagnosis of atopic dermatitis was considered. Medications (conjugated estrogens and atrovastatin) were withdrawn in order to rule out drug-induced pruritus. No improvement resulted. The patient's pruritus worsened despite treatment with antihistamines. Systemic steroids produced clinical improvement but relapse occurred after withdrawal of therapy. A thorough workup for generalized pruritus, including liver, renal, and thyroid function tests, bacteriology, and chest X-ray, was performed but rendered no relevant information. Positive patch-test results to Disperse Blue 106, 85, and 124 persisted for 3 weeks( Fig. 15). The pruritus appeared to be related to a hypersensitivity reaction to textile dyes and resins, and so the patient began to wear only white and beige cotton garments. By 1½ months, the pruritus was diminished and was completely resolved in 2 months.
Atopic dermatitis-like textile CD
Case 7.—A 10-year-old boy with suspected atopic dermatitis was referred to our clinic for investigation of environmental contact allergens. He had been suffering from pruritus on his palms, wrists, and shins for several months. The boy had participated in a soccer team for 3 years as a goal keeper. He had been wearing special gloves and shin shields consisting of an external hard plastic cover, rubber padding, and a dark textile lining on the inside, that came in contact with the skin. Lichenification on the wrists, shins, and popliteal areas was observed.
Patch testing with standard textile and rubber additive series, as well as extracts and pieces of the rubber part of the gloves and shields and parts of the textile lining was carried out. Hypersensitivity reactions occurred at the sites of the alcohol extracts of the textile and pieces of the black textile used in the lining. No hypersensitivity reactions were observed to any of the standard textile and colorsfinish allergens. The lesions resolved after changing the shield to another brand.
Discussion
Chronic subacute and acute dermatitis are the most frequent presentations of textile contact dermatitis according to previous studies.[2, 3, 4, 6] Erythematous patches with or without fine desquamation are a common form of textile dermatitis. Usually these lesions develop at sites where the garments fit tightly, such as inner and posterior thighs, popliteal fossae, buttocks, waistband area, and anterior and posterior axillary folds, sparing the vault (Figs. 16, 17). Textile dermatitis can also assume other clinical appearances that are atypical and thus delay the correct diagnosis of CD produced by clothing.
 |  |
| Figure 16 | Figure 17 |
|---|
Erythema-multiforme-like lesions can be an atypical manifestation of hypersensitivity to disperse dyes, as reported in the literature and observed in two of our patients.[8, 9, 10, 11] Erythema-multiforme-like CD related to hypersensitivity to the azo dye, Disperse blue 124, was reported even in a child.[12] In our cases, the erythema-multiforme-like CD lacked the typical target lesion and the histopathological findings resembled those of contact dermatitis, including the admixture of multiple eosinophils in the inflammatory infiltrate. In the first case, erythema-multiforme-like CD was provoked by exposure to two different types of allergens, nickel and azo dyes. This finding shows that erythema-multiforme-like reactions are not allergen specific but rather represent a pattern of response to delayed-type hypersensitivity to topical agents.
Purpuric CD related to hypersensitivity to textile dyes and resins has been previously described.[3, 13, 14, 15, 16, 17, 18] Although purpuric CD is not among the common clinical presentations of textile CD, it is not an atypical and extraordinary manifestation. In our experience, purpuric CD to clothing is more frequent than previously reported.[3, 19, 20] This phenomenon could be due in part to the climatic factors in Israel, where the hot and humid climate favors profuse sweating and thus enhances the exposure to the allergens.
Papular CD to textiles is a rare phenomenon. Follicular and papular lesions are reported in two patients with textile dermatitis causes by formaldehyde,[21] and a dermal reaction is noted with Disperse Blue 106.[22] It is of interest that in our patient the papular eruption also has purpuric features. The purpura is demonstrated histologically both in a lesional biopsy and in the biopsy from a positive patch test to Kaurit S. Admixture of purpura with papules is observed also in our patient with purpuric contact dermatitis (Case 3). Similar features of papules and purpura are described in the patients observed by Khanna.[23] It can be speculated that under certain circumstances strong allergens trigger an influx not only of lymphocytes but also of erythrocytes in the inflammatory infiltrate. Textile dermatitis with purpuric papules can resemble granuloma annulare, papular dermatitis, dermatitis herpetiformis, and mycosis fungoides and has to be differentiated from these entities.
Pigmented CD is an atypical manifestation of textile CD occasionally described in case reports.[25, 26, 27] Pigmented clothing dermatitis has been related to hypersensitivity to disperse dyes [3, 16, 18, 28] and to an azo dye coupling component agent, Naphthol AS.[29] In our case, the pigmented patches are pruritic and appear without previously discernible eczematous lesions, in contrast with the findings of Ancona Alayon et al.[29] In their series the Naphthol AS pigmented CD presents with spotted hyperpigmentation on the exposed areas but without pruritus. The hyperpigmentation is most pronounced in individuals with dark complexions, as we also observe. The histological features included melanocyte proliferation, incontinence of pigment, and various degrees of damage to the basal layer.
In the literature, phototoxic reactions to textiles[30] and contact depigmentation from the textile azo dye, Solvent Yellow 3, have been reported.[31]
Apart from fiberglass, which can contaminate clothes and induce irritant, pruritic, contact dermatitis,[33] pruritus and excoriations are seldom mentioned as a part of the clinical manifestation of clothing CD.[3, 33] Our patient demonstrates that pruritus and excoriation without dermatitis in the initial stages may also be a rare form of hypersensitivity to textile dyes and resins. Indeed she has undergone a thorough and expensive workup for generalized pruritus prior to patch testing.
Although intolerance to wool and synthetic fibers are well known in atopic dermatitis,[34] childhood atopic dermatitis-like, allergic, CD reactions with lichenification, related to hypersensitivity to textile dyes or resins, are not documented. Our patient displays the features of chronic dermatitis with lichenification at areas reminiscent of the distribution of lesions in atopic patients. The triggering agent in the incriminated textile cannot be defined, but the clinical course demonstrates the relevance of the suspected clothing.
Other unusual forms of textile dermatitis to dyes and resins described in the literature include pustular lesions[3] and large, erythematous patches with desquamation.[6] Textile CD presenting as lichen amyloidosis, with hyperkeratotic papules and plaques and positive patch tests to fragrance mix, formaldehyde, and formaldehyde resins has been described recently.[25]
Our series of patients with allergic textile contact dermatitis demonstrates the atypical and unusual clinical presentations of allergic contact dermatitis to clothing. It should be noted that apart from the well-delineated clinical forms such as EM-like contact dermatitis, pigmented contact dermatitis, pruritus, and excoriation, mixed forms including papular and purpuric lesions, and purpuric and pigmented lesions can be also present. Being familiar with the typical and unusual forms of textile contact dermatitis allows more rapid and precise diagnosis of clothing-related, contact dermatitis, which is not uncommon.
References
1. Hatch KL, Maibach HI. Textile dye allergic contact dermatitis prevalence. Contact Dermatitis 42:187-195, 2000.2. Pratt M, Taraska V. Disperse blue dyes 106 and 124 are common causes of textile dermatitis and should serve as screening allergens for this condition. Am J Contact Dermatitis 11:30-41, 2000.
3. Lazarov A, Trattner A, David M, Ingber A. Textile dermatitis in Israel: A retrospective study. Am J Contact Dermatitis 11:26-29, 2000.
4. Lazarov A, Trattner A, Abraham D, David M. Frequency of textile dye and resin sensitization in patients with contact dermatitis in Israel. Contact Dermatitis 46:119, 2002.
5. Uter W, Geier J, Lessmann H, Hausen B M. Contact allergy to Disperse Blue 106 and Disperse Blue 124 in German and Austrian patients, 1995 to 1999. Contact Dermatitis 44:173-177, 2001.
6. Seidenari S, Giusti F, Massone F, Mantovani L. Sensitization to disperse dyes in a patch test population over a five-year period, Am J Contact Dermatitis 13:101-108, 2002.
7. Marks J G, Belsito D V, De Leo V A et al. North American contact dermatitis group patch test results for the detection of delayed hypersensitivity to topical allergens. J Am Acad Dermatol 38:911-918, 1998.
8. Belsito DV. Textile dermatitis. Am J Contact Dermatitis 4:249-252, 1993.
9. Seidenari S, Di Nardo A, Motolese A, Pincelli C. Erythema multiforme associated with contact sensitization. Description of 6 clinical cases. G Ital Dermatol Venereol 125:35-40,1990.
10. Seidenari S, Manzini B M, Danese P. Contact sensitization to textile dyes: description of 100 subjects. Contact Dermatitis 24:253-258, 1991.
11. Pecquet C, Assier-Bonnet H, Artigou C, Verne-Fourment L, Saiag P. Atypical presentation of textile dye sensitization. Contact Dermatitis 40:51, 1999.
12. Baldari U, Alessandrini F, Raccagni AA. Diffuse erythema multiforme-like contact dermatitis caused by disperse blue 124 in a 2-year-old child. J Eur Acad Dermatol Venereol. 12:180-181, 1999.
13. Stewart WM. Lichenoid, pigmented and purpuric dermatitis of the lower extremities (wool, sweat and purpura). Ann Dermatol Syphiligr (Paris) 74: 661-662, 1967.
14. Batcschvarov B, Minkov DM. Dermatitis and purpura from rubber in clothing. Trans St Johns Hosp Dermatol Soc. 54:178-82, 1968.
15. Fisher AA. Purpuric contact dermatitis. Cutis 33(4): 346, 349, 351, 1984.
16. van der Veen JP, Neering H, de Haan P, Bruynzeel DP. Pigmented purpuric contact dermatitis due to Disperse Blue 85. Contact Dermatitis 19:222-223, 1988.
17. Foti C, Elia G, Filotico R, Angelini G. Purpuric clothing dermatitis due to Disperse Yellow 27. Contact Dermatitis 39: 273, 1998.
18. Komericki P, Abere W, Arbab E, Kovachevich Z, Kranke B. Pigmented purpuric contact dermatitis from Disperse Blue 106 and 124 dyes. J Am Acad Dermatol 45:456-8, 2001.
19. Lazarov A, Cordoba M. The purpuric patch test in patients with allergic dermatitis from azo dyes. Contact Dermatitis 42:23-6, 2000.
20. Lazarov A, Cordoba M. Purpuric contact dermatitis in patients with allergic reactions to textile dyes and resins. J Eur Acad Dermatol Venereol 42:23-26, 2000.
21. Uehara M. Follicular contact dermatitis due to formaldehyde. Dermatologica 156:48-54, 1978.
22. Dooms-Goosens A. Textile dye dermatitis. Contact Dermatitis 27: 321-323; 1992.
23. Khanna M, Sasseville D. Occupational contact dermatitis to textile dyes in airline personnel. Am J Contact Dermatitis 12: 208-210; 2001.
24. Trattner A, David M. Textile contact dermatitis presenting as lichen amyloidosus. Contact Dermatitis 42:107- 108, 2000.
25. Hayakawa R, Matsunaga K, Kojima S, Kaniwa M, Nakamura A. Pigmented contact dermatitis due to cotton flannel nightdress. Nippon Hifuka Gakkai Zasshi 95:1441-6, 1985.
26. Osmundsen PE, Larsen E. Pigmented contact dermatitis. Ugeskr Laeger 149:2856-2857,1987.
27. Valsecchi R, di Landro A, Pansera B, Cainelli T. Pigmented contact dermatitis. Contact Dermatitis 33:70-71, 1995.
28. Shah SA, Ormerod AD. Pigmented purpuric clothing dermatitis due to disperse dyes. Contact Dermatitis 43:360, 2000.
29. Ancona-Alayon A, Escobar-Marques R, Gonalez-Mendoza A, Bernal Tapia JA, Macotela-Ruiz E, Jurado-Mendoza J. Occupational pigmented contact dermatitis from Naphthol AS. Contact Dermatitis 2:129-34, 1976.
30. Hjorth N. Phototoxic textile dermatitis ("bikini dermatitis"). Arch Dermatology 112:445-1447, 1976.
31. Bajaj AK, Misra A, Misra K, Rastogi S. The azo dye Solvent Yellow produces depigmentation. 42:237-238, 2000.
32. Wang BJ, Lee JY, Wang RC. Fiberglass dermatitis: report of two cases. J Formos Med Assoc 92:755-8, 1993.
33. Veien NK, Hattel T, Laurberg G. Can "label dermatitis" become "creeping neurotic excoriations"? Contact Dermatitis 27:272-3, 1992.
34. Diepgen TL, Stabler A, Hornstein OP. Textile intolerance in atopic eczema. A controlled clinical study. Z Hautkr 65:907-10; 1990.
© 2003 Dermatology Online Journal

