Pseudoxanthoma elasticum
Published Web Location
https://doi.org/10.5070/D30fw8f41pMain Content
Pseudoxanthoma elasticum
Mercedes E Gonzalez MD, Henry J Votava MD, George Lipkin MD, Miguel Sanchez MD
Dermatology Online Journal 15 (8): 17
Department of Dermatology, New York UniversityAbstract
Pseudoxanthoma elasticum is an incurable, autosomal-recessive, genetic disorder that is caused by mutations in the ABCC6 gene. It is characterized by progressive mineralization and fragmentation of the elastic fibers in the skin, retina, and blood vessels. The characteristic cutaneous features bring the patient to medical attention, but morbidity is related to the degree of extracutaneous involvement. The disease is progressive with phenotypic variability and no definite genotype-phenotype correlation. Treatment is supportive and is directed at prevention and early detection of adverse ocular and cardiovascular sequelae. We present two siblings with pseudoxanthoma elasticum, who have considerable differences in disease related morbidity, which highlights intra-familiar phenotypic heterogeneity.
History
 |  |
| Figure 1 | Figure 2 |
|---|
 |
| Figure 3 |
|---|
Patient A is a 53-year-old man, who presented to the Dermatology Clinic at Bellevue Hospital Center for evaluation and treatment of numerous yellow, skin-colored papules on his neck that he initially noted in adolescence. Although the lesions are asymptomatic, he was seeking treatment to improve the appearance of these skin changes. Past medical history includes the presence of hypertension, diabetes mellitus, hyperlipidemia, obesity, and coronary artery disease. When he was 48 years old, he underwent coronary artery stent placement. Two years later he suffered two myocardial infarcts in a six-month period. At 53 years of age, he required a single coronary artery bypass graft. In addition to these coronary ischemic events, he has endured two strokes, with residual right arm weakness. He reports progressive loss of visual acuity due to angiod streaks on the lining of the retina and has required periodic ophthalmologic evaluation and intervention. Past medical history also includes a 40-pack-year cigarette smoking history, but he denies hematuria, gastrointestinal bleeding, claudication, or other skin disease. The patient is the youngest of six children. Three of his siblings as well as his paternal grandfather have similar skin and eye features.
Patient B is the eldest sister and is a 63-year-old woman, who noticed the appearance of grouped, yellow papules and linear plaques on her neck when she was 13 years old. Over time, new lesions developed in her axillae, flexural aspects of the elbows, and inguinal regions. Eighteen years ago, she underwent surgical excision of redundant skin folds. She also has progressive loss of central vision due to complications of her disease but denies a history of cardiovascular manifestations (stroke or myocardial infarcts), high blood pressure, diabetes mellitus, hematuria, gastrointestinal bleeding, claudication, or other cutaneous manifestations. She reported a past history of cigarette smoking.
Physical examination
In patient A, symmetrically distributed on the posterior and lateral aspects of the neck were many, 1 to 5 mm, yellow papules in a linear and reticulated pattern. The papules coalesced to form smooth-surfaced plaques. On the posterior aspect of the neck the skin was soft, lax, and wrinkled, with deep horizontal grooves and overhung folds.
In Patient B, on the anterior neck and axillae were numerous, small, smooth, well-demarcated, yellow papules that coalesced into linear, cobblestone-like plaques. The lesions impart the appearance of a plucked chicken's skin.
Laboratory data
In patient A, non-contrast computed tomography scan of the head showed lacunar infarction and suprasellar hyperdensities (calcifications). A bilateral carotid ultrasound showed right 1-49 percent stenosis and left 50-79 percent stenosis In patient B, laboratory studies are unavailable.
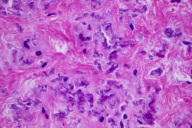
Histopathology
In the mid reticular dermis, there are accumulations of thick, curled, and irregularly clumped elastic fibers with calcification.
Comment
Psuedoxanthoma elasticum (PXE) is a rare genetic disorder that is characterized by progressive mineralization and fragmentation the of elastic fibers in the skin, eyes, and blood vessels. The condition is estimated to affect one in 50,000 to one in 70,000 people, with a female predominance [1]. The typical cutaneous features are small, yellow papules and plaques in a cobblestone or linear pattern that usually appear in late childhood or adolescence. With age and disease progression, the skin may become soft, lax, and wrinkled, which resembles plucked chicken skin. The most commonly affected sites are the neck, axillae, antecubital and popliteal fossae, and the periumbilical area. Papules on mucosal surfaces, which usually are on the inner aspect of the lower lip, can be observed. Dystrophic calcinosis cutis and cutis laxa are additional associations [2].
Although the skin lesions initially are the main concern of the patient, they are asymptomatic and mostly a cosmetic issue. Morbidity in PXE is due to the extracutaenous manifestations. In the eye, calcification of the elastin-rich membrane that lines the retinal epithelium, which is known as Bruch's membrane, leads to microscopic cracks, which are known as angioid streaks. At the site of these defects, fragile new blood vessels emerge that rupture with minor increases in pressure. As the disease progresses, recurrent episodes of retinal hemorrhages lead to central vision loss but preservation of peripheral vision [3]. Up to 40 percent of patients become blind. The eye findings, which are present in up to 85 percent of patients, are typically evident shortly after the appearance of the skin lesions [3]. Cardiovascular manifestations usually develop last and are the result of slowly progressive calcification and degeneration of the elastic fibers in arterial walls. These abnormalities can lead to decreased peripheral pulses, peripheral vascular occlusion, and claudication; hypertension from renal artery involvement; and coronary-artery disease with angina and/or myocardial infarcts. The fragility associated with calcified submucosal vessels may lead to gastrointestinal tract hemorrhage, which is the most important vascular complication of the disease. Less commonly, hemorrhages occur in the urinary tract or the brain.
Psuedoxanthoma elasticum is an autosomal recessive disorder, with considerable inter and intra-family phenotypic variability as demonstrated in the siblings above. This genetic variation may be explained by the presence of modifying genes and/or environmental factors [4]. However, overall phenotypic severity cannot be reliably correlated with the type and position of the mutation [5]. Nevertheless, carriers of a single mutant allele of the ABCC6 gene may have a subclinical phenotype and rarely can develop severe ophthalmologic and cardiovascular manifestations or demonstrate microscopic changes in the elastic fibers of the skin [6].
Psuedoxanthoma elasticum is caused by mutations in the ATP-binding cassette transporter C6 (ABCC6), which encodes for multidrug resistance-associated protein 6 (MRP6), which is a cellular transport protein. To date over 300 distinct mutations have been identified in PXE [1]. ATP-binding cassette transporter C6 is expressed at a very low level, or not at all, in the tissues affected by PXE [4]. Several theories have been proposed to explain this finding. The leading theory suggests that PXE is a metabolic disease and that defects in the ABCC6 transporter gene lead to the presence or absence of circulating factors that are normally needed to prevent aberrant mineralization in the elastic fibers under normal calcium phosphate homeostasis [8].
Major diagnostic criteria for PXE [9] include characteristic skin involvement, ocular findings, and the typical histopathologic features of clumped, calcified, and fragmented elastic fibers in the mid and deep dermis [10]. The differential diagnosis includes elastosis perforans serpiginosa, dermatofibrosis lenticularis (Buschke-Ollendorf syndrome), localized acquired cutaneous psuedoxanthoma elasticum, and Ehlers-Danlos syndrome.
There is still no universally effective treatment or cure for PXE. Although recent evidence suggests that dietary supplementation with oral phosphate binders and magnesium may alter the disease course [11, 12], treatment is still aimed at prevention and early detection of adverse ocular and cardiovascular complications. Early recognition of the characteristic cutaneous features with histopathologic confirmation is critical and can allow for timely surveillance. Patients should have frequent evaluations by a cardiologist and an ophthalmologist and should be counseled on reduction of cardiovascular risk factors, avoidance of platelet inhibitors, and activities that may increase the risk for bleeding.
References
1. Li Q, et al. Pseudoxanthoma elasticum: clinical phenotypes, molecular genetics and putative pathomechanisms. Exp Dermatol 2008; 18: 1 [PubMed]2. Federico A, et al. Dystrophic calcinosis cutis in pseudoxanthoma elasticum. J Am Acad Dermatol 2008; 58:707 [PubMed]
3. Hu X, et al. Pseudoxanthoma elasticum: a clinical, histopathological, and molecular update. Surv Opthalmol 2003; 48:424 [PubMed]
4. Uitto J, et al. Pseudoxanthoma elasticum-like phenotypes: more diseases than one. J Invest Dermatol 2007; 127:507 [PubMed]
5. Pfender EG, et al. Mutation detection in the ABCC6 gene and genotype-phenotype analysis in a large international case series affected by pseudoxanthoma elasticum. J Med Genet 2007; 44:621 [PubMed]
6. Martin L, et al. Heterozygosity for a single mutation in the ABCC6 gene may closely mimic PXE: consequences of this phenotype overlap for the definition of PXE. Arch Dermatol 2008; 144: 301 [PubMed]
7. Trip M, et al. Frequent mutation in the ABCC6 gene (R1141X) is associated with a strong increase in the prevalence of coronary artery disease. Circulation 2002; 106: 773 [PubMed]
8. Jiang Q, et al. Pseudoxanthoma elasticum is a metabolic disease. J Invest Dermatol 2009; 129: 348 [PubMed]
9. Lebwohl M, et al. Classification of pseudoxanthoma elasticum: report of a consensus conference. J Am Acad Dermatol 1994; 30:103 [PubMed]
10. Christen-Zach S, et al. Pseudoxanthoma elasticum: evaluation of diagnostic criteria based on molecular data. Br J Dermatol 2006; 155: 89 [PubMed]
11. LaRusso J, et al. Elevated dietary magnesium prevents connective tissue mineralization in a mouse model of pseudoxanthoma elasticum (Abcc6-/-). J Invest Dermatol 2009; 129(6):1388 [PubMed]
12. Sherer DW, et al. Oral phosphate binders in the treatment of pseudoxanthoma elasticum. J Am Acad Dermatol 2005; 53:610 [PubMed]
© 2009 Dermatology Online Journal

