Generalized linear porokeratosis: A rare entity with excellent response to acitretin
Published Web Location
https://doi.org/10.5070/D306x5w77kMain Content
Generalized linear porokeratosis: A rare entity with excellent response to acitretin
Taru Garg MD, Ramchander MD, Bincy Varghese MD, Meenu Barara MD, Anita Nangia MD
Dermatology Online Journal 17 (5): 3
Department of Dermatology & STD, Dermatology, Venereology & Leprosy, Lady Hardinge Medical College, New Delhi, India. chanderram41@gmail.comAbstract
Linear porokeratosis is a rare disorder of keratinization that usually presents at birth. We report a 17-year-old male with generalized linear porokeratosis, a very rare variant of porokeratosis, with extensive involvement of the trunk and extremities along with nail and genital involvement. The patient was treated with oral acitretin with excellent clinical response.
Introduction
Porokeratosis (PK) is a clonal disorder of keratinization characterized clinically by the presence of a hyperkeratotic ridge and histologically by a compact column of parakeratotic cells called the cornoid lamella.
Since its first description by Mibelli and Respighi in 1893, many new variants of porokeratosis have been described. Classically, five clinical variants are recognized: classic porokeratosis of Mibelli, disseminated superficial actinic porokeratosis (DSAP), disseminated superficial porokeratosis (DSP), porokeratosis palmaris et plantaris disseminata, and linear porokeratosis. Besides these, there are a few rare atypical morphological forms such as facial porokeratosis, giant porokeratosis, punched- out porokeratosis, hypertrophic verrucous porokeratosis and reticulate porokeratosis reported in the literature [1].
Linear porokeratosis is a distinctive variant of PK, which has further been classified into localized and generalized forms based upon the distribution of lesions. Very few cases of generalized linear porokeratosis have been described in the literature [2, 3, 4, 5]. We report here yet another case of this very rare variant, an adolescent male with extensive disfiguring lesions and unusual features, who showed a dramatic clinical response to oral acitretin.
Case report
A 17-year-old male born of a non-consanguineous marriage presented with widespread hyperpigmented, papules and plaques since 5 years of age. The lesions first appeared on the dorsum of the left hand and progressively increased to involve the arms, the trunk, and the left leg. The lesions were asymptomatic and consultation was primarily sought for cosmetic reasons.
 |  |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Lesions of generalized linear porokeratosis involving the trunk and upper extremities Figure 2. Involvement of hands and nails by generalized linear porokeratosis | |
On examination there were numerous linear and whorled, hyperpigmented annular scaly plaques of variable shapes and sizes along the lines of Blaschko distributed on the trunk, both upper limbs and the left leg (Figures 1 and 2).
 |
| Figure 3 |
|---|
| Figure 3. Close up view of an individual lesion showing raised thready margins and furrowing |
Papules and plaques showed mild central atrophy and raised thready margins with furrowing (Figure 3). Linear lesions were also present on the palms, but soles were spared. There was significant flexural involvement in the form of lesions in right axilla, left groin, right retro-auricular groove and natal cleft. A few scattered lesions on the neck, left external auditory canal and right leg were also noted. Genital involvement was also marked with characteristic lesions present on the penile shaft and scrotum. Depigmented plaques with peripheral keratotic ridges were present on the glans and prepuce in a linear pattern. Fingernails showed longitudinal ridging and distal splitting. The face, scalp, and oral mucosa were spared.
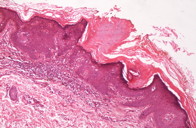
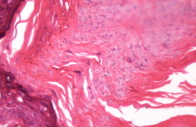
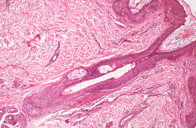
Biopsy from the edge of the lesion showed the presence of basket weave orthokeratosis in the epidermis. The occasional hair follicles noted were unremarkable. The edge of the biopsy showed the presence of a superficial keratotic plug with a central column of parakeratosis. The base of the parakeratotic plug showed reduced thickness of the granular layer (Figures 4 and 5).
The eccrine acrosyringia and hair follicles appeared normal without any overlying cornoid lamellae (Figure 6).
The patient was started on acitretin at a dose of 0.5 mg/kg body weight. After 6 weeks of therapy marked flattening of lesions was observed (Figure 7).
After 5 months of treatment all the lesions had flattened but failed to clear completely (Figures 8 and 9). Residual hyperpigmentation was observed in the affected areas.
Discussion
Although porokeratosis as an entity has been known for more than a century the exact pathogenesis of the disorder still remains an enigma. It is regarded as an autosomal dominant disorder with variable penetrance. It is suggested that when an autosomal dominant disorder occurs in a mosaic arrangement the lesions may be particularly severe. In such cases the segmental involvement may be superimposed on a more diffuse involvement. Mosaicism can also explain the occurrence of skin lesions in a linear distribution in PK [6]. Three loci on chromosome 12p, 15q25 and1p31.3-p31 have been associated with PK [7]. Genetic susceptibility, sun exposure, viral etiology (especially Hepatitis B and C viruses, HIV), and immunosuppresion have all been proposed to play a role in triggering the clonal proliferation of keratinocytes. Linear porokeratosis differs from other variants in that it frequently manifests at birth or early childhood and has a high risk of developing malignancies especially Bowen disease and squamous cell carcinoma.
The association between porokeratosis and cutaneous malignancy is well documented. Chromosomal instability and reduced immune surveillance with overexpression of p53 are hypothesized to play a role in the development of cutaneous malignancies within porokeratosis. It is found that 7.5 percent of porokeratosis patients develop a skin malignancy in their lifetime. The risk factors associated with development of malignant change include long-standing lesions, increasing age, linear type of porokeratosis, and presence of large lesions on extremities [8].
Generalized linear prokeratosis is a very rare variant of porokeratosis and is characterized by the presence of multiple, often large plaques, involving the trunk as well as the extremities as observed in our case. Here we would like to highlight certain peculiarities in our patient, which include extensive involvement of the trunk and extremities, involvement of flexures in addition to the other sites, and nail and genital involvement. The simultaneous occurrence of all these unusual features in an affected individual is a very rare occurrence.
Linear porokeratosis needs to be differentiated from another important entity designated as “porokeratotic adnexal ostial nevus” (PAON). PAON includes both porokeratotic eccrine and hair follicle nevus (PEHFN) and porokeratotic eccrine ostial and dermal duct nevus (PEODDN) [9]. There is some overlap in the clinical findings of linear porokeratosis and PAON. Widespread PAON usually presents at birth with erythema and blistering. Multiple keratotic comedo-like lesions in linear or band-like arrangementmay be seen. Our case, on the other hand, manifested lesions in early childhood without any history of redness or blistering. Besides, thread-like elevated rims of hyperkeratosis that are the clinical correlates of cornoid lamellae were conspicuous in our case. This furrowing is not appreciated in cases of PAON and is a useful marker for clinical differentiation. Further, the histological hallmark of PAON is a cornoid lamellae overlying dilated and hyperplastic eccrine ostia and/or hair follicles. The characteristic clinical morphology of the lesions and the absence of adnexal involvement in our case favors a diagnosis of generalized linear PK rather than PAON.
Various treatments have been reported to be beneficial in patients with porokeratosis including 5-fluorouracil, imiquimod, retinoids, and the destructive modalities (such as cryotherapy, CO2 laser, curettage, excision, and dermabrasion). Prior to the removal of etretinate from the US market, conflicting reports of etretinate efficacy were published. Etretinate at doses of 75 mg/day for 1 week followed by 50 mg/day was shown to be helpful in linear porokeratosis and symptomatic porokeratosis of Mibelli. Higher doses of 1 mg/kg/day were reported to exacerbate lesions of DSAP after 4-6 weeks of treatment [10]. Acitretin, a second-generation monoaromatic retinoid produced a good response in a case of systematized linear porokeratosis [11].
The age of the patient, the extensive involvement, and the disfiguring nature of the lesions along with the high risk of malignancy prompted us to give a trial of oral acitretin in this patient. The initial response was encouraging and after 5 months of treatment the lesions resolved almost completely except for those on the dorsum of the hands and the palms, which seemed to be relatively refractory to treatment. The patient is on regular follow up and we plan to treat the patient with intermittent courses of acitretin. As for the resistant lesions we plan to treat these with topical 5-flourouracil.
Even though the strides made in eliciting the exact pathogenesis of this disorder of keratinization in recent years are quite impressive, treatment continues to be challenging. There are no defined protocols regarding the use of retinoids in porokeratosis, especially linear porokeratosis, in which the risk of malignancy is a serious concern. Long-term follow up of such patients is therefore of utmost importance and any suspicious looking lesions need to be biopsied and treated promptly.
References
1. Palleschi GM, Torchia D. Porokeratosis of Mibelli and superficial disseminated porokeratosis. J Cutan Pathol 2008; 35:253-5. [PubMed]2. Rahbari H, Cordero AA & Mehregan AH. Linear porokeratosis: A clinical variant of porokeratosis of Mibelli. Arch Dermatol 1974; 109: 526-528. [PubMed]
3. Goldman GD, Milstone LM. Generalized linear porokeratosis treated with etretinate. Arch Dermatol 1995; 131(4):496-7. [PubMed]
4. Ersoy L, Koc K, et al. A case of generalised linear porokeratosis. Turkderm 1997; 31: 190-191.
5. Dervis E, Demirkesen C. Generalized linear porokeratosis. Int J Dermatol 2006; 45 (9): 1077 – 1079. [PubMed]
6. Happle R. Segmental forms of autosomal dominant skin disorders: different types of severity reflect different states of zygosity. Am J Med Genet 1996; 66: 241-2. [PubMed]
7. Liu P, Zhang S, et al. Identification of a genetic locus for autosomal dominant disseminated superficial actinic porokeratosis on chromosome 1p31.3-p31.1.Hum Genet. 2008; 123(5):507-13. [PubMed]
8. Sasson M, Krain AD. Porokeratosis and cutaneous malignancy. A review. Dermatol Surg. 1996; 22(4):339-42. [PubMed]
9. Goddard DS, Rogers M, et al. Widespread porokeratotic adnexal ostial nevus: clinical features and proposal of a new name unifying porokeratotic eccrine ostial and dermal duct nevus and porokeratotic eccrine and hair follicle nevus. J Am Acad Dermatol. 2009; 61(6):1060.e1-14. [PubMed]
10. Knobler RM, Neumann RA. Exacerbation of porokeratosis during etretinate therapy. Acta Derm Venereol. 1990; 70(4):319-22. [PubMed]
11. Hong JB, Hsiao CH, Chu CY. Systematized linear porokeratosis: a rare variant of diffuse porokeratosis with good response to systemic acitretin. J Am Acad Dermatol. Apr 2009; 60(4):713-5. [PubMed]
© 2011 Dermatology Online Journal