 |
 |
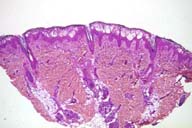
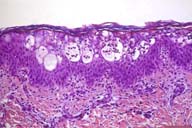
| Figure 3 | Figure 4 |
|---|---|
| Skin biopsy demonstrating marked edema of the upper epidermis | Epidermal spongiosis and an eosinophil-rich cellular infiltrate |
Histologically, there is spongiosis manifest as epidermal intercellular edema with exocytosis of numerous eosinophils and mononuclear cells both within the epidermis as well as in spongiotic foci. Dyskeratotic keratinocytes are present adjacent to spongiotic microvesicles. An interstitial infiltrate of lymphocytes and eosinophils is present in the papillary dermis.
Incontinentia pigmenti is an X-linked dominant disorder that presents in at or soon after birth. Although the condition involves the skin primarily, there are a number of associated disorders including dental defects, convulsive disorders, mental retardation, ocular abnormalities and childhood neoplasms. Because it is almost always lethal in males, is observed almost exclusively in female infants.
Three successive stages of the cutaneous disease have been described. The first stage is characterized by a linear, erythematous, vesiculobullous eruption on the trunk and extremities within the first 2 weeks of life.[2] Histologically, spongiosis containing numerous eosoinophils with abundant dyskeratotic keratinocytes is noted.[1,3] The second stage, the so-called verrucous stage, usually develops within a few weeks and is manifest as verrucous hyperkeratotic papules and plaques. [2] Microscopically, there is acanthosis, papillomatosis, and hyperkeratosis with abundant dyskeratotic cells, often in small whorls in the epidermis.[3] Vacuolar change of the basal layer may be noted. Finally, as lesions resolve, the hyperpigmented stage develops in which there is a whorled slate-gray to brown hyperpigmentation that usually fades with time.[2] These areas contain many melanophages in the upper dermis.[3]
The most characteristic histologic features of the vesicular stage are spongiosis in which there are numerous eosinophils, eosinophils in the epidermis and dyskeratotic keratinocytes. The term "eosinophilic spongiosis" is a histologic reaction pattern that refers to the presence of spongiosis with eosinophils in the epidermis. It may be seen in a number of different conditions including allergic contact dermatitis, bullous pemphigoid and insect bite reactions.[1] Dyskeratotic keratinocytes are seen in relatively few disorders such as lichen planus, erythema multiforme and drug eruptions. Although the two most impressive histologic findings are non-specific, the presence of numerous dyskeratotic keratinocytes, often in clusters, in association with spongiotic dermatitis in an infant is virtually diagnostic of incontinentia pigmenti.[1,3]
This infant had classic findings of the vesicular stage of IP.
Although linear vesiculobullous lesions on the extremities of a female newborn are suggestive of incontinentia pigmenti, the clinical differential diagnosis of blistering lesions in a newborn should be considered. Bullous lesions are known to occur in congenital syphilis (so-called pemphigus syphiliticus), usually on the palms and soles. These infants are usually born premature and are ill-appearing, and may have other features such as syphilitic rhinitis, wrinkled skin, a papular eruption, and deep fissures of the oral commisures and lateral nares.[4] Congenital herpes simplex can mimic incontinentia pigmenti, and both the inherited and the infectious disease may occur simultaneously.[5] Other infectious diseases, such as congenital varicella, neonatal and congenital candidiasis, and staphylococcal infection must also be excluded. Acropustulosis of infancy is a chronic and relapsing vesiculopustular disroder that also may resemble incontinentia pigmenti initially.[2] Linearity of bullae in incontinentia pigmenti, especially in the presence of verrucous lesions, is a helpful distinguishing feature. Although an infant form of pemphigoid may cause both a histologic and clinical diagnostic dilemma, other heritable blistering diseases of the newborn such as epidermolysis bullosa or herpes gestationis can be more easily differentiated. Rarely, acrodermatitis enteropathica may look similar to incontinentia pigmenti and congenital syphilis.
As expected, she progressed through the second and third stages although many patients do not. This case is an excellent one in that it demonstrates the importance of clinicopathologic correlation in the accurate diagnosis of a rarely encountered disorder.