

Figure 2. Broad, aseptate hyphae (KOH)
Cutaneous mucormycosis is an uncommon disease and occurs mainly in immunocompromised patients. We report an immunocompetent infant who developed primary cutaneous mucormycosis at an intravenous line site secured with an arm board and elastic bandage. The isolate was identified as the zygomycete, Rhizopus sp. High mortality rates are reported with invasive mucormycosis; however, early identification of the causative agent and antifungal therapy led to complete cure of the lesions in the reported case.
 |
 |
| Figure 1 | Figure 2 |
|---|---|
| Figure 1. Erythematous plaque with vesicles on the right dorsal forearm Figure 2. Broad, aseptate hyphae (KOH) |
|
 |
 |
| Figure 3 | Figure 4 |
|---|---|
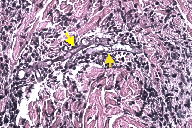
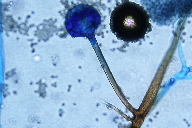
| Figure 3. Yellow arrows pointing at broad, aseptate hyphae on the papillary dermis (H&E) Figure 4. Unbranched sporangiospores with rhizoids directly underneath |
|
A 6-month-old female infant was admitted to the pediatric ward for pneumonia. She was the product of an uncomplicated full term pregnancy. Her past medical history was unremarkable. She was in perfect health without preceding recurrent infections. There was no known family history of immunodeficiency. A diagnosis of bacterial pneumonia was made based on lobar consolidation seen on plain chest films. Blood cultures were negative. An intravenous line was placed on the right wrist to initiate intravenous antibiotic treatment and the line was secured with an arm board and bandage. A vesicular eruption, several centimeters proximal to the catheter site, was found on day 3 of admission (Figure 1). The vesicles were sampled for examination with potassium hydroxide (Figure 2) and a biopsy specimen was taken from the site (Figure 3). Tissue culture revealed the organism shown on Figure 4.
Mucormycoses are infections by fungal species of the order Mucorales, family Mucoraceae, and class Zygomycetes that infect a wide range of patients and have a high capacity for causing severe disease and even death. The most severe infections are typically among immunocompromised adults, but children and patients with no underlying medical conditions also contract life-threatening infections [1]. The most frequent presentation of mucormycosis is rhinocerebral mucormycosis in diabetic patients with ketoacidosis [1, 2]. The incidence of cutaneous mucormycosis varies among reports, ranging from 10 to 19 percent of all cases of fungal infections [1, 2]. Mucormycosis in children is most prevalent among those who are born prematurely, have low birth weight, are receiving therapy with corticosteroids or broad-spectrum antibiotics, are afflicted with diarrhea and/or malnutrition, or have local skin trauma [1, 3]. Additionally, pediatric cases of cutaneous mucormycosis have been associated with wooden tongue depressors, cotton stockingettes, and adhesive bandages [3, 4].
Cutaneous mucormycosis has two common presentations, which many regard as different stages in the progression of disease rather than two distinct entities [2, 3, 4]. Its evolution is slow, developing over the course of days, differentiating it from rapidly progressing infections associated with Clostridium perfringens or Group A Streptococcus [3]. Superficial cutaneous mucormycosis begins as an erythematous patch, initially resembling phlebitis [2]. Vesicles and pustules develop on this erythematous patch and may progress to ulceration and eschar formation. Cutaneous disease in immunocompetent patients is typically limited to this superficial presentation. Gangrenous cutaneous mucormycosis is characterized by progression to a black, necrotic area with surrounding erythema [3].
Cutaneous mucormycosis, especially gangrenous, can disseminate to other tissues and organs. A case review by Roden, et al. revealed that 43 of the 176 cases of cutaneous mucormycosis reported in English literature had deep extensions to tendon, muscle, or bone. Thirty-five of the 176 cases spread hematogenously to other organs [1].
The diagnosis of cutaneous mucormycosis can be difficult and a high degree of suspicion is imperative to allow prompt identification and initiation of treatment. Identification of a fungus from tissue culture can be made in 24 hours, but speciation may take a week. The most common genera eventually identified are Mucor, Rhizopus, and Absidia [2]. Because wound cultures take time and blood cultures are generally negative, microscopy is the key to making the diagnosis of cutaneous mucormycosis. As demonstrated in the presented case, microscopy with potassium hydroxide prep of the lesion is an expeditious way to identify branching fungal hyphae. H&E stain of tissue samples can support the diagnosis by showing irregularly shaped, broad, non/pauci-septate hyphae with right-angle branching [2, 4]. Histologically demonstrated invasion of subcutaneous tissues and blood vessels is indicative of gangrenous cutaneous mucormycosis [3].
Prompt treatment is imperative in preventing morbidity associated with mucormycoses [3]; therefore, treatment should not be withheld pending culture results. Systemic amphotericin (1-1.5 mg/kg/day) is the mainstay of treatment with debridement being an important adjunct therapy for gangrenous cutaneous mucormycosis [1, 3, 4]. Posaconazole is a promising alternative to amphotericin, but its use and appropriate dosing has not been established in children.
Overall, mortality related to mucormycoses is high. The high mortality rate associated with mucormycoses may be due to the underlying immunodeficiencies in patients who contract these infections. A case review looking specifically at upper extremity cutaneous mucormycosis revealed that whereas there was a high incidence of amputation, there were no deaths among immunocompetent patients with this infection [2]. Among the 929 cases reviewed by Roden, et al., there was a 57-70 percent survival rate among patients who received treatment with amphotericin, surgical debridement, or both, and only a 3 percent survival rate among those patients who received no treatment for their fungal infection. Disseminated cutaneous mucormycosis had a 95 percent mortality rate [1]. In a series of 18 infants with cutaneous mucormycosis, the survival rate was reported to be approximately 39 percent [3].
This case illustrated several key concepts regarding cutaneous mucormycosis. The diagnosis was quickly established by potassium hydroxide prep of vesicules and later confirmed by tissue biopsy and culture. The prompt initiation of therapy resulted in complete recovery and spared the patient from potentially disfiguring surgical debridement. An investigation for underlying immunodeficiencies should be considered in patients with mucormycosis, especially in pediatric patients. An immunologic work-up performed on our patient revealed no immunodeficiency. The patient was in perfect health at follow-up one year later. The case reported herein is a good illustration of primary cutaneous mucormycosis resulting from local skin trauma, likely from a contaminated arm board and bandage.
© 2010 Dermatology Online Journal