
A 46-year-old male patient presented with hyperpigmented verrucous plaques and papules mainly on the left cheek and malar region that had evolved over a 7 month period. Histopathology demonstrated the presence of a large number of classical copper penny bodies or muriform bodies and a predominantly neutrophilic dermal infiltrate that confirmed the diagnosis of chromoblastomycosis.
 |
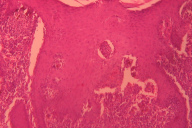
| Figure 1 |
|---|
A 46-year-old male patient presented with hyper-pigmented verrucous plaques and papules mainly on the left cheek and malar region for the last seven months (Figure 1). There was no history of injury prior to the onset of the lesion. Initially, an asymptomatic erythematous papule appeared and this slowly increased in size and became verrucous. Later, a few more papules appeared around the larger plaque. The lesions had an eythematous border that gradually merged with the surrounding normal skin. There was no history of ulceration or discharge. Lymph nodes were not palpable. The patient had been previously treated with systemic antibiotics and topical steroids without much improvement. He did not have any systemic complaints. A routine blood count and chemistry panel were within normal limits. An incisional biopsy was done and the histopathological findings are shown in Figures 2 and 3.
 |
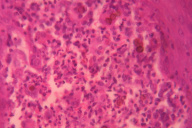 |
| Figure 2 | Figure 3 |
|---|
Routine H & E staining showed pseudo-epitheliomatous hyperplasia of the epidermis and a predominantly neutrophilic infiltration in the dermis with focal areas of microabscess formation. Many golden-brown thick-walled round structures were seen representing sclerotic bodies.
Our patient was a middle-aged man who presented to us with an asymptomatic slowly growing verrucous plaque. Our initial diagnosis included cutaneous tuberculosis and atypical mycobacterial infection. However, histopathology study demonstrated the presence of a huge number of classical copper penny bodies or muriform bodies and a predominantly neutrophilic dermal infiltrate confirmed the diagnosis of chromoblastomycosis. We started the patient on itraconazole 200 mg daily and planned for regular follow-up. Unfortunately, the patient was lost to follow up in the very first month of the commencement of therapy.
Chromoblastomycosis is a chronic fungal infection of the skin and subcutaneous tissue. Five species of dermatophyte fungi, Fonsecaea pedrosoi, Fonsecaea compactum, Cladosporium carrionii, Phialophora verrucosum and Phialophora dermatitidis, are the main causative agents of this disease [1]. It is primarily a disease of tropical or subtropical regions like Africa, the West Indies, South America, and India, mainly in persons working outdoors in agricultural occupations; it is thus reported most commonly in men. The infection usually results from trauma such as a puncture from a wood splinter [2].
Carrion described five types of lesions in a case of chromoblastomycosis-nodules, tumors, plaques, warty lesions, and scarring lesions [3]. The disease spreads in the adjacent skin with characteristic satellite lesions surrounding the primary source. Metastatic spread to other organs is reported in a minority of cases [4].
Chromoblastomycosis usually occurs on the hands, feet, and legs. In the present case, the primary involvement of the face was unusual. Pradhan et al. found that involvement of extremities accounts for more than 90 percent of the cases of chromoblastomycosis [5]. There are very few reported cases of involvement of the face [6]. Other unusual sites mentioned in the literature are the nasal ala, ear, penile shaft, vulva, tracheolaryngeal region, tonsil, ileocecal region, and pleural cavity [7].
The diagnosis of chromoblastomycosis is based on KOH examination, identification of organism in histological sections, and culture of the organism that reveals slowly growing green to black colonies. The microscopic appearance of the conidia formation identifies the species [8].
Treatment of chromoblastomycosis is difficult and not well established. Small lesions can be treated by simple surgical excision with large margins followed by systemic treatment with an oral antifungal drug to avoid dissemination. Usually, itraconazole (200-400 mg/day orally for 6 months) is the treatment of choice, with an 80-90 percent rate of success [9]. Clinical and biologic cure has been reported in mild to moderate disease after a mean duration of therapy of 7.2 months with itraconazole alone [10]. A combination of fortnightly liquid nitrogen cryotherapy and pulsed monthly itraconazole (200 mg twice daily for 7 days per month) is more cost-effective and shortens the duration of therapy compared with the use of itraconazole or cryotherapy alone [11]. The combinations of itraconazole with 5 fluocytosine or amphotericin B were found synergistic for F. pedrosoi by an in vitro susceptibility study [12]. Terbinafine, fluconazole, ketoconazole, and thiabendazole have been used with a reasonable amount of success. Intravenous amphotericin B (up to 1 mg/kg daily) is recommended in extensive cases [9]. Voriconazole and posaconazole efficacy is being tested [13]. Topical heat [14], cryotherapy [15], and CO2-laser ablation [16] also have been described as treatment options.
Our case was unique because of its unusual site of presentation and the absence of any trauma prior to onset. Although chromoblastomycosis is very rare on the face, our case demonstrates the need for consideration of chromoblastomycosis in the differential diagnosis in treatment-resistant verrucous plaques of the face.
© 2010 Dermatology Online Journal