Unknown: Pedunculated nodule on the foot
Paulo Morais MD1, Marcos Guimarães MD2, Aurea Canelhas MD2, Filomena Azevedo MD1
Dermatology Online Journal 18 (4): 5
1. Department of Dermatology and Venereology
2. Department of Pathology
Hospital S. João EPE; Faculty of Medicine, University of Porto, Porto, Portugal
Abstract
Eccrine poroma is a benign adnexal neoplasm composed of epithelial cells with poroid or distal ductal differentiation. We
report a healthy 57-year-old woman with a 4-year history of an asymptomatic pedunculated nodule on the lateral border of the
right foot that was proven to be an eccrine poroma by histopathologic examination.
Answer: Eccrine poroma
History
An otherwise healthy 57-year-old woman presented with a 4-year history of a pedunculated nodule on the lateral border of the
right foot. The growth had slowly enlarged over the years. The patient denied any previous local trauma or significant pain,
except when wearing closed shoes. Physical examination revealed a 30 x 28 x 12 mm non-tender, flesh-colored, pedunculated
firm nodule with a hyperkeratotic surface that protruded from the border of her right foot (Figure 1).
 |
 |
| Figure 1 |
Figure 2 |
Figure 1. Clinical appearance of the patient. (A) Lateral view; (B) dorsal view. Note the presence of a well-demarcated erythematous
plaque surrounding the lesion that disappeared about a week after excision of the lesion, probably representing a reactive
inflammatory process.
Figure 2. Histological image (H&E stain) of the tumor showing anastomosing strands of uniform, small, cuboidal, epithelial
cells with monomorphous ovoid nuclei, inconspicuous nucleoli, and a moderate amount of pale eosinophilic cytoplasm, without
atypia or mitosis (A, magnification x20). These cells were continuous with the basal layer of the epidermis and extended into
the upper dermis. Note the presence of small ducts throughout the lesion (B, arrow head, magnification x100), occasional cysts
(C, asterisk, magnification x20), and dilated vessels (D, arrow, magnification x100). |
The lesion was excised and the specimen was submitted for histopathologic study (Figure 2).
Case presentation
 |
| Figure 3 |
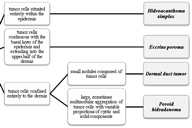
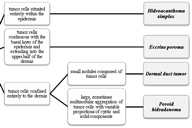
| Figure 3. Subtypes of poroma according to Ackerman [1]. The differentiation between subtypes is mainly based on the location of the tumor cells. There are some cases with 2 or
more histopathological variants. Therefore, it is sometimes difficult to demarcate sharply among the variants. |
The term “poroma” refers to a group of benign adnexal neoplasms with “poroid” or tubular (usually distal ductal) differentiation [1]. The malignant variant of EP, porocarcinoma, is a far less common entity [2]. Like syringoma, poroma has been interpreted historically as a neoplasm of eccrine lineage, mostly because of enzyme histochemical
findings of doubtful specificity [3]. Types of poromas include the typical eccrine poroma (EP) as well as its three distinct histological subtypes (Figure 3).
These subtypes display varying cellular growth patterns as follows: hidroacanthoma simplex, dermal duct tumor, and poroid
hidradenoma [1]. However, more recently it has been suggested that poromas can be a proliferation of either eccrine or apocrine lineage
[4]. The difficulty in differentiating both lineages of poromas occurs because the sweat ducts of the two are histologically
and immunohistochemically identical. The term acrospiroma is used by some authorities as a synonym for poroma and is used
by others as a broad designation that includes both poroma and hidradenoma.
First reported by Pinkus et al in 1956 [5], EPs are believed to comprise 10 percent of all sweat gland tumors, which of themselves represent only 1 percent of all
primary cutaneous lesions [6, 7]. The pathogenesis of EP is unknown, although it has been associated with scarring, trauma, and radiation [8, 9]. There is no predilection according to race or sex. It tends to be diagnosed in patients aged from 40-70 years [10]. The most common location is on the foot (47%), although cases have been described on the head, trunk, and upper limbs [1, 7, 8]. Clinical diagnosis of EPs is often difficult because they exhibit a polymorphic gross appearance and may mimic lesions
as diverse as pyogenic granulomas, skin tags, warts, cysts, and other adnexal tumors. Although they usually present as skin-colored
papules, plaques, or nodules less than 2 cm in diameter, pigmented poromas (from melanin), and erythematous lesions (from
dilation or proliferation of blood vessels) have been reported [6, 8]. Surface erosion or ulceration, presumably secondary to trauma, are occasionally reported.
Histologically, EP consists of a circumscribed proliferation of compact cuboidal keratinocytes with small monomorphous nuclei
and scant eosinophilic cytoplasm. The degree of ductal differentiation varies greatly in individual neoplasms but is evident
in most EPs [6, 8]. Carcinoembryonic antigen (CEA) immuperoxidase staining, which labels the luminal surface of both apocrine and eccrine ducts,
can be employed to confirm the presence of ductal differentiation. Poromas can be confined to the epidermis (intraepidermal
poroma, or hidroacanthoma simplex), can occur in broad continuity with the epidermis, with extension into the papillary dermis
(juxtaepidermal poroma), or can develop wholly (or nearly so) within the dermis (intradermal poroma or dermal duct tumor)
[1, 6, 8]. At times, a poroma may display striking clear cell change and may rarely display small foci of necrosis en masse or coagulation
necrosis. These features are not of any known clinical significance and, in this case, necrosis en masse is not a clue to
a malignancy. In addition, some poromas are accompanied by cystic spaces in the epidermis, hyperkeratosis at the surface of
the tumor, or foci of sebaceous differentiation, usually consisting of clusters of mature sebocytes near the lesion base and
presumably representing apocrine poromas [11]. Rarely, multiple poromas will develop, either in an acral or in widespread distribution, a clinical pattern referred to
as poromatosis [12].
The diagnosis of EP typically cannot be made based exclusively on clinical findings, although experienced clinicians may recognize
the entity. The dermoscopic features of pigmented and nonpigmented EPs have recently been described [7, 13]. Pigmented poromas mimic a number of skin tumors, including pigmented basal cell carcinomas, seborrheic keratosis, and malignant
melanoma, because they present with various clinical, dermoscopic, and histopathological features [13]. In the case of nonpigmented EP, dermoscopic analysis can help in the differential diagnosis, although neither clinical
findings nor dermoscopy can guarantee that we can distinguish such lesions from amelanotic melanoma, porocarcinoma, or squamous
cell carcinoma [7]. Therefore, the diagnosis of EP is only fully established after surgical excision with subsequent microscopic examination
by a trained dermatopathologist.
The prognosis of EPs is good because the lesions have no known clinical significance. Although it is possible that a significant
proportion of eccrine porocarcinomas follows a preexisting EP, which undergoes malignant transformation [1, 14], this risk is minimal and is thought to be similar to that of normal skin.
References
1. Ackerman AB. Poromas. In: Abenoza P, Ackerman AB (eds): Neoplasms with eccrine differentiation. Philadelphia: Lea & Febiger, 1990:113-185.
2. Kazakov DV, Kutzner H, Spagnolo DV, et al. Sebaceous differentiation in poroid neoplasms: report of 11 cases, including
a case of metaplastic carcinoma associated with apocrine poroma (sarcomatoid apocrine porocarcinoma). Am J Dermatopathol 2008;30:21-26. [PubMed]
3. Hashimoto K, Lever WF. Histogenesis of skin appendage tumors. Arch Dermatol 1969;100:356-369. [PubMed]
4. Harvell JD, Kerschmann RL, LeBoit PE. Eccrine or apocrine poroma? Six poromas with divergent adnexal differentiation. Am J Dermatopathol 1996;18:1-9. [PubMed]
5. Pinkus H, Rogin J, Goldman P. Eccrine poroma: tumors exhibiting features of the epidermal sweat duct unit. Arch Dermatol 1956;74:511-521. [PubMed]
6. Pylyser K, Wolf-Peters C, Marien K. Histology of eccrine poromas: study of 14 cases. Dermatologica 1983;167:243-249. [PubMed]
7. Avilés-Izquierdo JA, Velázquez-Tarjuelo D, Lecona-Echevarría M, Lázaro-Ochaita P. Dermoscopic Features of Eccrine Poroma.
Actas Dermosifiliogr 2009;100:133-136. [PubMed]
8. Hyman AB, Brownstein MH. Eccrine poroma. An analysis of forty-five new cases. Dermatologica 1969;138:29-38. [PubMed]
9. Nemoto I, Akiyama N, Aoyagi S, Nomura T, Shimizu H. Eccrine porocarcinoma and eccrine poroma arising in a scar. Br J Dermatol 2004;150:1232-1233. [PubMed]
10. Moore TO, Orman HL, Orman SK, Helm KF. Poromas of the head and neck. J Am Acad Dermatol 2001;44:48-52. [PubMed]
11. Lee NH, Lee SH, Ahn SK. Apocrine poroma with sebaceous differentiation. Am J Dermatopathol 2000;22:261-263. [PubMed]
12. Navi D, Fung M, Lynch PJ. Poromatosis: the occurrence of multiple eccrine poromas. Dermatol Online J 2008;14:3. [PubMed]
13. Minagawa A, Koga H. Dermoscopy of pigmented poromas. Dermatology 2010;221:78-83. [PubMed]
14. Robson A, Greene J, Ansari N, et al. Eccrine porocarcinoma (malignant eccrine poroma): a clinicopathologic study of 69
cases. Am J Surg Pathol 2001;25:710-720. [PubMed]
© 2012 Dermatology Online Journal