
A 12-year-old girl presented with a 2-year history of a 10 cm area of asymptomatic brown coalescent plaques of coalescent, linearly arranged papules on the lower back. No other physical or systemic abnormality was detected. Routine laboratory investigations, including thyroid function tests, were normal. The histopathological examination revealed hyperkeratosis, papillomatosis, and elongated rete ridges in the epidermis. On special staining (Alcian blue), mucin deposition was seen in the papillary dermis. The remaining dermis was normal. A diagnosis of Mucinous Nevus was made.
 |
 |
| Figure 1 | Figure 2 |
|---|---|
 |
| Figure 3 |
|---|
A 12-year-old girl presented with multiple, asymptomatic brown plaques on the lower back, with 2 years of evolution (Figure 1). These plaques progressively enlarged and increased in number. The patient was otherwise healthy and had received no treatment before coming to our clinic.
On physical examination, we observed multiple brown plaques made up of coalescent, linearly arranged papules on the lower back. The plaques were soft, compressible and well-defined, with a zosteriform distribution. There was no history of antecedent trauma to the area or family history of similar lesions. No other physical or systemic abnormality was detected. Routine laboratory investigations including thyroid function tests and protein electrophoresis were normal.
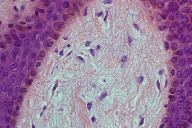
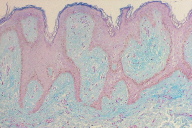
A biopsy of the lesion was performed and the histopathological examination revealed hyperkeratosis, papillomatosis, and elongated rete ridges in the epidermis (Figure 2). On special staining (Alcian blue), mucin deposition was seen in the papillary dermis (Figure 3). The remaining dermis was normal.
Mucinous nevus (MN) is a rare form of primary cutaneous mucinosis. In the revision of the literature we found only 12 cases of MN, being described by the first time in 1993 by Redondo-Bellon et al. [1] The term mucinous nevus was proposed because of its nevoid appearance and characteristic pattern of mucin deposits in the papillary dermis. It is considered a benign hamartoma that can be congenital or acquired. It may be divided into two histopathologic types: connective tissue nevus of the proteoglycan (CTNP) and combined epidermal-CTNP [2]. Half of the cases can be assigned to the CTNP type and the other half to the combined epidermal-CTNP type.
The lesions usually develop at birth [1] or in early adulthood [3, 4], and the lower part of the trunk is the most commonly affected site. Mucinous nevus consists of a papular plaque, usually in a unilateral linear nevoid pattern. Brakman et al. and Rongioletti and Rebora reported two adult cases of linear mucinous nevus on the back, showing a zosteriform pattern [3, 4].
The histopathology in all cases designated as mucinous nevus includes a papillary dermal mucin deposit with or without elongated rete ridges in a band like fashion [1]. As mucin staining gives a positive reaction with Alcian blue at pH 2.5, but is negative at pH 0.5, the mucin in the lesion is thought to be composed of hyaluronic acid [4]. The origin of the mucin deposited in the lesion remains unclear, but it seems to be the result of a primary metabolic process (overproduction) rather than of a secondary catabolic process [5]. This idea is supported by the fact that in all reported cases the lesions developed early in life, even at birth, without evidence of trauma or a pre-existing pathological change at the site of the lesions.
Clinically it must be distinguished from epidermal nevus, connective tissue nevus, nevus lipomatosus superficialis and other superficial hamartomas, as well as from other forms of cutaneous mucinosis, such as the cutaneous mucinosis of infancy, the cutaneous focal mucinosis, and the papular mucinosis.
In conclusion, this case is being reported for its rarity. Because of the benign nature of the lesions, MN does not require therapy, except for aesthetic purposes. Recently, Chi et al. [2] proposed that carbon dioxide laser vaporization may be a treatment option for mucinous nevus of the combined epidermal-CTNP type with multiple lesions but not for the CTNP type.
© 2010 Dermatology Online Journal