This is a case of classic type Kaposi sarcoma occurring in an 85-year-old woman who presented with indurated vascular plaques on both legs below the knee that has been present for two years. A brief review of the literature on Kaposi sarcoma is included.
 |
| Figure 1 |
|---|
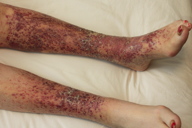
| Figure 1. Clinical photograph |
An 85-year-old woman presented with indurated vascular plaques on both legs below the knee (Figure 1) present for two years. She has been told in the past that it was stasis dermatitis. The lesions and associated mild pruritus had not responded to applications of fluocinonide cream. The patient’s past medical history included breast cancer treated by lumpectomy, hypertension, hypothyroidism, and gout. There was no history of immunodeficiency disease or hereditary cancer and she denied having other family members with similar cutaneous lesions. She had lived in Omaha her entire life. Physical examination revealed purple, indurated plaques limited to the skin below the knees. There were no similar lesions anywhere else on the body. There was no evidence of stasis edema about the feet and ankles or any associated lymphadenopathy.
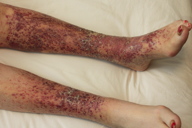
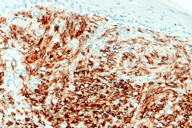
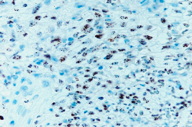
The lesion was biopsied and histopatholoic examination revealed a proliferative vascular neoplasm involving the entire dermis (Figures 2 and 3). The infiltrating spindled neoplastic cells were mixed with abnormal slits and vascular structures with red cell extravasation in the dermal stroma. Vascular marker CD34 was strongly positive (Figure 4). On immunostaining for HHV-8 (human herpes virus-8), there were numerous positive neoplastic spindle cell nuclei with a stippled dot pattern, a diagnostic finding for Kaposi sarcoma (Figure 5).
 |
 |
| Figure 4 | Figure 5 |
|---|---|
| Figure 4. Strongly positive dermal vessels on CD34 immunostaining. Figure 5. HHV-8 immunostaining shows positive nuclei with a stippled dot pattern. |
|
This case demonstrates an unusual presentation of classic Kaposi sarcoma in an elderly woman not of Eastern European or Mediterranean descent. Therapeutic options were considered, including intravenous and intralesional chemotherapy as well as treatment with interferon-alpha and radiation therapy. Because of the patient’s advanced age, relative lack of symptoms, and good functional status, the decision was made to defer treatment. Watchful waiting with clinical follow-up was deemed the appropriate treatment course.
The cutaneous nodules and related internal lesions of Kaposi sarcoma (KS) were first described in 1872 by Moritz Kaposi, a Hungarian dermatologist at the University of Vienna. For close to a century, KS was subsequently known as a rare disease characteristically seen in older men of Eastern European, Mediterranean, or Jewish descent. It was not until the 1980s when KS was found in approximately 40 percent of American men with AIDS that it was identified as an AIDS-defining illness [1]. With recent advances in the treatment of HIV, namely highly active antiretroviral therapy (HAART), the incidence of AIDS-associated KS has decreased dramatically in western countries.
The viral cause of KS was established in 1994, when human herpesvirus 8 (HHV-8), otherwise known as KS-associated herpesvirus (KSHV), was identified in close to 100 percent of all KS lesions. Based on the latest research, it is now believed that HHV-8 is necessary but not sufficient to cause KS. Other factors are required, the most significant being immunosupression. The mechanisms by which HHV-8 causes KS are not well understood, but a number of molecular events involving evasion of the immune system are implicated. The literature remains unclear as to whether KS is considered to be a virus-induced proliferation or a true malignancy, or both [1, 3].
There are four recognized forms of KS: classic KS, epidemic (AIDS-associated) KS, iatrogenic (transplant-associated) KS, and endemic (African) KS. Classic KS typically affects white males of Eastern European, Mediterranean, or Jewish origin between the fourth to eighth decades of life. Epidemic KS is associated with AIDS and is the most common malignancy associated with HIV infection [4]. Iatrogenic KS is usually found in transplant patients receiving immunosuppressive therapy and usually remits once immunosuppression is reversed. Endemic KS accounts for 10 percent of adult malignancies in Africa and typically affects a younger population [3]. Although the clinical manifestations of the four subtypes are reasonably consistent, their clinical courses vary.
Classic KS typically follows an indolent course, and patients often present with discrete erythematous or violaceous patches on the lower extremities that can evolve into plaques and nodules, which may ulcerate. It has an overwhelming male predominance with a male-to-female ratio of approximately 10-15:1. The incidence of classic KS in the United States has been estimated to be 0.34 for men and 0.08 for women per 100,000 per year [3]. Whereas the prevalence of classic KS in the United States and United Kingdom is low, higher rates are found in Italy, Greece, Turkey, and Israel. Although classic KS is considered to be a more benign form of the disease, AIDS-associated KS tends to be more aggressive and can be life-threatening if left untreated. In AIDS-associated KS, the lesions usually appear first on the upper body, head and neck, and then progress to internal structures, with the most common sites being the lungs, gastrointestinal tract, and lymph nodes [4].
Histologically, skin biopsies of KS show abnormal spindle cell proliferation with vascular slits and vascular structures with prominent endothelial cells in the dermis. Extravasated erythrocytes and hemosiderin-laden macrophages are seen. Some spindle cells may show nuclear pleomorphism and mitosis. KS in its earlier stages may resemble granulation tissue with a diffuse chronic inflammatory infiltrate [5]. Immunohistochemical staining for HHV-8 shows stippled dots in the nuclei of the spindle cells and is diagnostic for KS. The spindle cells of KS are also positive for CD34 and Factor VII immunostains. The origin of the spindle cell, the hallmark of KS, is unknown. The literature favors a lymphatic or vascular endothelial cell precursor [6].
The differential diagnosis of KS includes entities such as pyogenic granuloma, other vascular tumors, bacillary angiomatosis, and pseudo-KS, namely severe stasis dermatitis. Pseudo-KS, otherwise known as acral angiodermatitis, is a benign angiomatous proliferation commonly associated with chronic venous stasis [3]. Whereas this may resemble KS histologically, the characteristic narrow vascular slits of KS are usually absent and CD34 staining is negative. Clinically, KS is divided into three main subtypes, localized nodular disease, locally aggressive disease, and generalized KS. For patients with localized nodular disease or iatrogenic KS related to reversible immune suppression, the prognosis is excellent. Locally aggressive KS has a 3-year survival rate of 64 percent, but generalized KS is usually fatal within three years if left untreated [3].
The treatment of KS depends on disease progression, clinical type, and immune status. There is no gold standard therapy for KS, but current guidelines emphasize treating effectively without immunocompromising the patient. Therapeutic interventions include surgical excision and laser therapy for localized cutaneous or mucosal disease. Topical 0.1 percent alitretinoin gel is FDA approved for discrete skin lesions. Radiation therapy shows good response rates and produces symptomatic relief. Chemotherapy with agents such as vinblastine, bleomycin, and liposomal anthracyclines including doxorubicin and daunorubicin, and paclitaxel is indicated for patients with more disseminated disease. Intralesional chemotherapy with vinblastine is also available for KS confined to the skin or mucosa. Interferon-alpha is now FDA-approved for systemic administration in patients with slowly progressive but extensive cutaneous disease. Many experimental treatment options, including anti-angiogenic, hormonal, and anti-viral agents, are currently being investigated [4].
© 2012 Dermatology Online Journal