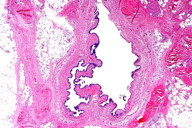
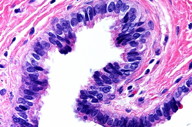
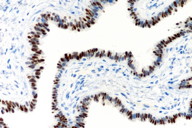
Figure 2. Note the cilia on the luminal border of the columnar epithelium.
An excisional biopsy of an asymptomatic cystic lesion that had been present for several years on the right heel of a 48-year-old woman revealed a subcutaneous cyst lined by ciliated columnar epithelium. On immunostaining, the epithelial cells were positive for Pan-cytokeratin (CK AE 1/3), estrogen receptor (ER) and progesterone receptor (PR), but negative for carcinoembryonic antigen (CEA), suggesting Mullerian type of epithelium. Cutaneous ciliated cyst of Mullerian type occurs almost exclusively on the lower extremity of premenopausal women. The lesion is benign and excision is curative.
These are the microscopic images from an excisional biopsy of an asymptomatic cystic lesion that had been present for several years on the right heel of a 48-year-old woman.
 |
 |
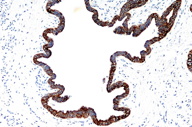
| Figure 3 | Figure 4 |
|---|---|
| Figure 3. Pan-CK (CK AE 1/3): Positive cytoplasmic cytokeratin immunostain. Figure 4. CEA immunostaining: Negative. |
|
 |
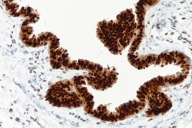 |
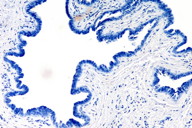
| Figure 5 | Figure 6 |
|---|---|
| Figure 5. ER (Estrogen Receptor) immunostain: Positive nuclear stain. Figure 6. PR (Progesterone Receptor) immunostain: Positve nuclear stain. |
|
Cutaneous ciliated cyst (CCC) is a rare solitary cystic lesion occurring on the lower limb of women, typically in the younger, pre-menopausal years of life [1-6]. Histologically, CCC is an unencapsulated dermal and/or subcutaneous unilocular or multilocular cyst, with variable surrounding fibroadipose tissue, resembling fallopian tube (minus the muscular wall). Cyst walls are lined by cuboidal to columnar ciliated epithelium, occasionally pseudostratified, and often arranged in papillary projections. Areas of squamous metaplasia can be seen, but there is an absence of skin appendages [1]. Lack of mucin producing cells is the rule [1].
Most favor a Mullerian origin for CCC, presumably from sequestered portions of the paramesonephros in the developing lower limb buds [3, 4, 5, 6]. Evidence for a Mullerian origin for CCC include the strong association with the female gender, location on lower limbs, frequent growth during reproductive years, and the Estrogen Receptor (ER) and Progesterone Receptor (PR) positivity [3, 6]. Others have suggested ciliated metaplasia of sweat glands as a possible alternative etiology of CCC [1, 5]. CCC, however, lacks connection with adnexal structures [1, 6] and has an immunohistochemical profile more in keeping with fallopian tube, including positivity for ER, PR, and negativity with CEA and GCDFP-15, whereas the reverse pattern is true for eccrine glands [3]. In addition, eccrine glands in human skin show a much broader distribution than just the lower limb [3], by far the most predominant site for CCC[1]. Futhermore, the myoepithelial layer typical of sweat glands is lacking in CCC [3, 6]. Lastly, cilia in CCC, like those of the fallopian tube, are of the ultrastructural 9+2 type, whereas the cilia seen in fetal eccrine ducts and eccrine tumors are of 9+0 type [1, 3, 4, 6]. Indeed, cutaneous Mullerian cyst [3, 5, 6] has been offered as a preferred name over CCC to reflect that ciliated epithelium can line other cutaneous cysts such as bronchogenic cyst, thyroglossal duct cyst, branchial cleft cyst, thymic cyst, perianal caudal gut cyst, and vulvar cyst [2, 3, 4]. Lee et al concluded that the rare cases of CCC occurring in males and in unusual locations such as scalp are thought to arise from ciliated metaplasia of eccrine or apocrine glands, based on the fact that many of these cases are CEA positive and show evidence of a myoepithelial layer [5].
The differential diagnosis of cutaneous ciliated cyst/cutaneous Mullerian cyst (CCC/CMC) includes other cutaneous cysts capable of showing cilia, namely, bronchogenic cyst, branchial cleft cyst, thymic cyst, thyroglossal duct cyst, vulvar cyst, perianal (caudal gut) cyst, and cutaneous endosalpingiosis [2]. Unlike CCC/CMC, bronchogenic cysts occur in the thorax and neck region and typically also show goblet cells [2]. Branchial cleft cysts are located laterally in the neck, unlike CCC/CMC, and often show a lymphocytic infiltrate [2]. Thymic cysts will be differentiated from CCC/CMC by their location in the neck and presence of Hassall corpuscles [2]. Thyroglossal duct cysts are located in the midline of neck and may be associated with a sinus tract and thyroid follicles. The characteristic location of vulvar cyst along with the mucin-producing, endocervical-like epithelium typical of this entity easily distinguishes it from CCC/CMC. In fact, vulvar cyst may be a variant of Mullerian cyst, because vulvar cysts are also presumably of Mullerian origin [2]. Perianal (caudal gut) cysts are located in the perineum and they contain goblet cells and mucous glands, unlike CCC/CMC [2]. Cutaneous endosalpingiosis usually occurs in the context of an abdominal scar [2]. The presence of cilia, the absence of keratin in the cyst cavity, and the lack of appendageal structures helps distinguish CCC/CMC from other more common cutaneous cysts such as epidermal cyst, pilar cyst, steatocystoma, and hidrocystoma.
Cutaneous ciliated cyst is a benign lesion, first described by Hess in 1890 [1] and later named CCC by Farmer and Helwig [1]. Cutaneous Mullerian cyst (CMC) is a term preferred by some over CCC [3, 5, 6] because of its presumed Mullerian origin and to prevent confusion with other skin cysts showing cilia [2, 3, 4]. CCC/CMC often enlarges and becomes clinically apparent during hormonally active years and is cured by excision [3, 5]. Careful attention to clinicopathologic features help distinguish it from other ciliated cysts of the skin.
© 2011 Dermatology Online Journal