
A 67-year-old man presented with a complaint of a painful nodule on his back for approximately two months. On exam, a violaceous, firm, warm, indurated nodule measuring 3.5 x 2 cm was observed. Nine months prior to presentation, he was diagnosed with a moderately differentiated squamous cell carcinoma (SCC) of the left upper lobe (stage 1b), which was removed via video-assisted thoracoscopic wedge resection. Diagnosis of metastatic SCC secondary to traumatic seeding at a trocar port site was made. To our knowledge, this has not been previously described in the literature.
 |
| Figure 1 |
|---|
| Figure 1. Clinical picture of patient. A violaceous, non-mobile nodule measuring 3.5 x 2 cm in the infrascapular region |
A 67-year-old man presented with a complaint of a nodule on his back for approximately two months. On physical exam, a violaceous, warm, indurated, non-mobile, painful nodule measuring 3.5 x 2 cm was observed in the left infrascapular region (Figure 1).
Nine months prior to presentation, he was diagnosed with a moderately differentiated squamous cell carcinoma (SCC) of the left upper lobe, pT2NxMx, stage 1b. The tumor was removed via video-assisted thoracoscopic (VATS) wedge resection. Past medical history was also significant for severe idiopathic pulmonary fibrosis, hypertension, hyperlipidemia, and a 112.5 pack/year smoking history.
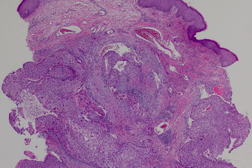
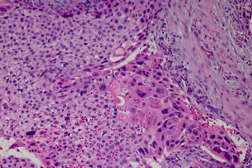
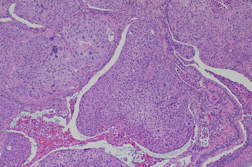
A specimen was submitted for histopathologic examination (Figure 2 and 3).
 |
 |
| Figure 2 | Figure 3 |
|---|---|
| Figures 2 and 3. Low and high power of skin lesion demonstrating multiple dermal islands of keratinizing epithelium embedded in a fibrous stroma. | |
Biopsy of the lesion revealed multiple dermal islands of keratinizing epithelium embedded in a fibrous stoma with epidermal attachment. Histology was similar to that of the patient’s lung carcinoma (Figure 4).
 |
| Figure 4 |
|---|
| Figure 4. High power image of patient’s primary squamous cell carcinoma of the lung. Islands of keratinizing epithelium can be appreciated within the respiratory epithelium |
At the time of his presentation to dermatology, the patient’s stage 1 lung cancer was managed conservatively. Follow up PET scans obtained 3 and 6 months after initial diagnosis of cancer were notable for increased metabolic activity at the trocar ports sites. This activity was attributed to post-surgical inflammation.
Based on our dermatological diagnosis, another PET-CT scan was ordered. This study revealed increased metabolic activity in the left hilum and anterior mediastinum, with extension into the chest wall, left ribs, and subcutaneous tissue. The patient was subsequently treated with chemotherapy. He died less than two weeks after his first infusion.
Although cutaneous metastases from the lung are rare, they must be ruled out in patients with suspicious skin lesions and a history of smoking or lung cancer. It is estimated that approximately 1 to 12 percent of patients with lung cancer develop cutaneous metastases [1]. These metastases have been described in the literature as being nodular, mobile or fixed, single or multiple, and painless. Common locations include the anterior chest, abdomen, back, and head/neck. Less commonly, lung metastases to skin may also present as papular, plaque-like, zosteriform, ulcerated, or erysipelas-like lesions. Erysipelas-like metastases may mimic true infections locally [1, 2]. In our case, the pain and warmth associated with the patient’s nodule raised the suspicion of a furuncle, abscess, or another infectious process.
Histologically, lung metastases to skin are usually moderately or poorly differentiated. Metastatic adenocarcinoma from the lung may show well-differentiated glandular structures and/or intracytoplasmic mucin. Squamous cell carcinomas metastatic to the skin are usually located within the dermis and/or subcutaneous fat. Islands of keratinizing epithelium may be observed with no connection to the epidermis. Small-cell carcinomas are generally anaplastic and have hyperchromatic nuclei with little cytoplasm. Lastly, large cell carcinomas present as undifferentiated tumors with large cells [1].
This case is unique in that an SCC of the lung metastasized to the skin via direct seeding through a VATS trocar port. VATS is a well-established technique for the diagnosis and treatment of thoracic malignancies. However, the procedure is occasionally associated with serious complications. Mechanisms implicated in possible port site involvement include direct contact of the chest wall with tumor during extraction, contamination of instruments, and residual pleural fluid in the chest cavity [3]. To date, only one study by Pareskh et al at Memorial Sloan Kettering Cancer Center has quantified the incidence of port site recurrences. In their analysis of 410 cases over a four-year period, only one port site recurrence (incidence rate of 0.26%) was identified [3].
Treatment of solitary cutaneous metastases may include surgery alone or in combination with chemotherapy and/or radiation [1]. Unfortunately, cutaneous lung metastases carry a poor prognosis with a mean survival of 3-7 months [2, 4].
© 2012 Dermatology Online Journal