
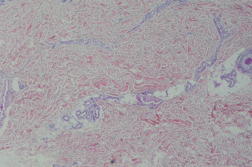
We report a 42-year-old woman with an asymptomatic solitary targetoid patch on her shin of 1 month duration. Histopathologic evaluation revealed intact epidermis with vascular proliferation in the papillary dermis. Vascular channels were irregular, thin walled, and dilated. They were lined by prominent endothelial cells having plumped protruding nuclei and scanty cytoplasm. There was a mild extravasation of red blood cells and mild lymphocytic infiltration around blood vessels in the upper and mid dermis.
 |
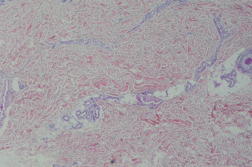 |
| Figure 1 | Figure 2 |
|---|---|
| Figure 2. Hobnail hemangioma: vascular proliferation in the papillary dermis (H&E x40) | |
Hobnail hemangioma, previously termed targetoid hemosiderotic hemangioma, is a form of benign vascular neoplasm that was first described by Santa Cruz and Aronberg in 1988 [1]. It usually presents as a solitary small, single lesion on the trunk and extremities (particularly in lower extremities) and less commonly on neck, head, oral cavity, breast, and buttock, in young to middle-aged patients (most frequently in 20s or 30s) [2, 3]. The typical form of hobnail hemangioma is more often seen in males than females but episodically changing hobnail hemangiomas have been described more in females than in males [4].
Clinical presentation is variable. Hobnail hemangioma sometimes presents as angiomatous or pigmented, nontargetoid, flat, or exophytic. However, in some cases it initially presents as a small purple papule, about two to three mm in diameter. Thereafter, an ecchymotic brownish ring appears and surrounds it, expands, and then later disappears spontaneously. In later stages, only the central papule persists. Its color is thought to relate to deposition of hemosiderin and extravasation of red blood cells. Most often the lesion is asymptomatic, but sometimes it can be painful [5].
The pathogenesis of hobnail hemangioma is unknown. Some authors postulate that hobnail hemangioma may develop from a preexisting hemangioma after trauma. There are other theories that trauma, radiation, pregnancy, and hormonal changes can trigger hobnail hemangioma. Some authors suggest a lymphatic origin for this skin problem [6]. According to its immunophenotype, such as expression of D2-40, lack of expression of CD34, and actin-labeled pericytes it has a pattern similar to lymphangioma [7]. Also there are some reports of cyclic clinical variations of hobnail hemangioma during menstrual cycles in women [4].
Histologically, hobail hemangioma is a poorly circumscribed vascular growth with a biphasic pattern. Superficially in the papillay dermis, dilated thin-walled vessels surrounded by a layer of endothelial cells with epithelioid or hobnail cells are exhibioted. Papillary projections and Fibrin thrombi are also seen within some vessels without endothelial multilayering or tufting. In the deeper dermis, there are small, slit-like, and angulated vascular spaces. The vessels have a collagen-dissecting pattern. There is also extravasation of RBCs hemosiderin deposits, and fibrosis in the surrounding stroma [3, 4].
It is important to differentiate hobnail hemangioma from malignant conditions such as Kaposi sarcoma, angiosarcoma, and melanoma. Histologic and dermatoscopic evaluation can be helpful to determine the correct diagnosis. For example, angiosarcoma can be ruled out with lack of histopathologic atypia. In addition, Hobnail Hemangioma does not have HHV-8 positive plasma cells, which are characteristic of Kaposi sarcoma [8].
No medical treatment is needed for Hobnail Hemangioma because it is not an infection or malignant process. Simple excision is possible for cosmetic or diagnostic reasons or if the growths are painful.
© 2012 Dermatology Online Journal