

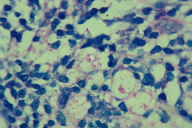
A 65-year-old man presented with an approximately 5-year history of cutaneous nodules of the arms and legs. In addition, physical examination revealed bilateral thickening of ulnar and tibial nerves, distal weakness with hallux extension and finger abduction, and distal hypoesthesia of the left hallux. Histopathological analysis of the skin biopsy specimen showed a dense inflammatory infiltrate in the hypodermis, characterized by vacuolated macrophages containing multiple organisms. The Fite stain was positive confirming the diagnosis of multibacillary leprosy.
Answer: Lepromatous leprosy
 |
 |
| Figure 1 | Figure 2 |
|---|
 |
 |
| Figure 3 | Figure 4 |
|---|
Lepromatous leprosy is a form of chronic granulomatous disease that is caused by the obligate intracellular organism, Mycobacterium leprae, which mainly affects the skin and peripheral nerves [1]. With early intervention, leprosy is a curable disease; however, if not recognized and treated promptly, permanent sequelae and disability result, mainly of the skin, peripheral nerves, and nasal mucosa [2].
The WHO classifies patients as paucibacillary (PB) if there are five or fewer skin lesions, or multibacillary (MB) if there are six or more skin lesions or if a skin smear is positive. The Ridley-Jopling scale ranks leprosy as indeterminate leprosy, tuberculoid leprosy, borderline tuberculoid leprosy, borderline leprosy, borderline lepromatous leprosy, and lepromatous leprosy [3].
Some important physical findings of lepromatous leprosy include polymorphic lesions, macules, papules and nodules, which can cover large areas with a symmetrical distribution. Ichthyosis on the legs, which can become ulcerated, thickening of nerves, madarosis, nasal mucosa and facial infiltration (leonine facies), ocular involvement [4] and hypogonadism are all complicatons [5].
Three main signs are the basis for the clinical diagnosis of leprosy: anesthetic skin lesions, enlarged peripheral nerves, and acid-fast bacilli in the skin smear. The presence of just one of them is sufficient for the diagnosis of leprosy. In this particular case, the skin smear result was negative, which is not that unusual because its sensitivity is low and varies from 10-50 percent, despite the fact that the specificity of skin smears is almost 100 percent [6]. Even though histopathological analysis has a higher sensitivity than skin smear [7], it is not required for diagnosis.
Since the beginning of the 1980s, WHO has been recommending multidrug therapy (MTD) to treat leprosy. MTD regimens for adult patients with MB disease consist of 50 mg of clofazimine and 100 mg of dapsone on a daily basis plus monthly doses of 600 mg of rifampicin and 300 mg of clofazimine. The regimen should be continued for 24 months.
For patients between 10 and 14 years old, the MB treatment consists of 50 mg of clofazimine every other day and 50 mg of dapsone on a daily basis, plus monthly doses of 450mg of rifampicin and 150 mg of clofazimine. Alternatively and for children younger than 10, the dose must be adjusted according to body weight. Dapsone is given daily at 2 mg/kg and clofazimine is given daily at 1 mg/kg. Monthly, rifampicin is added at 10 mg/kg and clofazimine at 6 mg/kg. The treatment duration is the same as for adults [8].
In Brazil, the country where this case was reported, in accordance with Ministry of Health data, 39,921 new cases were detected in 2007. Of these, 21,442 were of the MB type, reaching a rate of 21.08/100,000. Although the disease is found throughout country, the region known as Legal Amazon, in which resides only 12.9 percent of the Brazilian population, is the region with the biggest number of new cases detected in Brazil (38.9%). The difficult access to health services in this area caused by physical and social barriers, contributes to the maintenance of the endemic [9].
In accordance with the 2008 WHO report, the number of cases tracked around the world throughout 2007 went down from 252,525 to 212,802, showing a 4 percent decrease. Despite that, the disease is also still endemic in some areas of Angola, Central African Republic, Democratic Republic of Congo, India, Madagascar, Mozambique, Nepal, and the United Republic of Tanzania [10].
© 2009 Dermatology Online Journal