
(answer from unknown)
 |
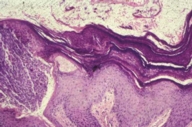 |
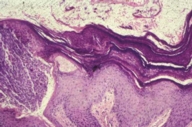
| Figure 1 | Figure 2 |
|---|
Histopathology showed a thickened stratum corneum, compact parakeratosis with retention of keratohyalin granules, vascular proliferation, and ectasia.
After the biopsy, the patient was recommended to apply Polysporin every day to the biopsy site. When she returned 2 weeks later for suture removal, the eruption had completely cleared.
Axillary granular parakeratosis is a clinicopathologic diagnosis first described by Northcutt et al. in 1991 [1]. Patients typically present with a pruritic axillary eruption of well-demarcated brownish-red, hyperkeratotic patches or papules that may be unilateral or bilateral. There is generally a history of deodorant use that often correlates with fluctuations in disease severity. Since the original description by Northcutt et al., there have been reports of similar disease occurring in other locations such as the submammary [2, 3] and intermammary region [2], groin [2], and abdomen [2]. Therefore, intertriginous granular parakeratosis [4] as well as granular parakeratosis [2] have been proposed as new names for this disorder. This disease is found more commonly in females in the fifth or sixth decade of life. However, there have recently been reports of pediatric cases with involvement in the diaper region [5].
Several theories have been proposed for the etiology of this disease. Because it has an axillary distribution, Northcutt et al. [1] and Mehregan et al. [6] proposed an allergic contact dermatitis to deodorant. In addition, they suggested that this external stimulus induced an error in epidermal differentiation [1, 6]. Arguments against an allergic contact reaction are the unilateral distribution, absence of an inciting agent, and lack of change with discontinuation of deodorant in some patients. Because the eruption was limited to moist regions of the body, Mehregan et al. theorized that mechanical irritation caused secondary changes in the skin [4].
Clinical differential diagnosis includes Hailey-Hailey disease, nummular eczema, or Bowen disease [1]. Definitive diagnosis is determined by biopsy. Histopathology reveals a unique compact parakeratosis with retention of basophilic keratohyalin granules within a markedly thickened stratum corneum.
A variety of treatment options have been reported to be successful. Isotretinoin [7], topical steroids [1, 6], tacalcitol [3] (a vitamin D analog), and cryotherapy [1] have been used with resolution of disease. Simple discontinuation of the presumed inciting topical agent has also resulted in clearance of the skin eruption in some cases [2, 8]. Spontaneous resolution has also been described [2, 5].
© 2005 Dermatology Online Journal