

Figure 1B: The region improved by the end of the 1 month of treatment.
A 7-year-old boy presented to our clinic with the complaint of dermatitis on the left eyelid and periorbital region. He had never had any similar lesions on his skin. He was a healthy boy with normal growth percentiles. None of his family members had a history of similar disease. This lesion developed 3 weeks after his brother scratched his eyelid. The remaining areas of the skin were normal. On physical exam, a sharply-demarcated, erythematous plaque with silvery white scale was present on the left eyelid and periorbital region (Fig. 1A). The nails were not involved.
 |
| Figure 2 |
|---|
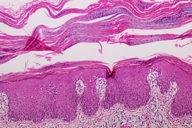
| Figure 2: Histopathologic examination showing elongation of rete ridge, absent granular layer, parakeratosis with neutrophils and dilated tortuous vessels in the dermal papillae (HEx20). |
A biopsy specimen was taken from the lesion, and histopathological examination revealed elongation of the rete ridge, absent granular layer, parakeratosis with neutrophils, and dilated tortuous vessels in the dermal papillae. A PAS stain to identify fungal infection was negative (Fig. 2). No hyphae or spores were observed in a scraping prepared with 20 percent KOH solution. Fungal and standard bacterial cultures from the skin lesion were negative. The clinical and histopathologic findings confirmed the diagnosis of psoriasis. The patient was treated with a topical corticosteroid twice daily for 1 month and was clear at that time (Fig. 1B). No relapse was observed during the followup period of 2 years.
Psoriasis of the eyelids is uncommon, as are other forms of facial psoriasis except eyebrows and hairline. Chronic ultraviolet radiation exposure may be a reason for facial sparing. One must conclude that other factors account for eyelid sparing in the majority of cases because the eyelids are usually shaded [1]. Other factors such as relative humidity may play a role. Many of the patients reported were improved in summer despite dense heavy fog and clothing; this suggests that environmental factors other than direct sun exposure contribute to seasonal fluctuation of the disease [2].
Various triggers for facial psoriasis include abrasions, bites, burns, contusions, excoriations, phototoxic reactions, pressure, tape stripping, and irritant application [1]. We think that trauma was the leading cause of psoriasis in the present case.
Fullerton and Orenberg have shown that facial involvement is associated with major forms of disease [2]. According to these authors, when the first lesion is present on elbows, knees, limbs or scalp, the patient is less likely to develop severe disease. However, when the first episode is facial, truncal, or extensive, severe psoriasis is more likely. They also concluded that even minor outbreaks on the face correlated with a generally severe affliction. Bernhard also suggested that such facial involvement is a marker of severe disease [1, 3]. For example, patients with well-defined, clear-cut psoriatic plaques on the cheeks often have psoriasis that is more severe than patients without facial involvement in terms of extent of involvement elsewhere on the body; their psoriasis may be recalcitrant to treatment and have a tendency to relapse after treatment. Psoriasis of the eyelids has similar implications. In a retrospective study by Morris et al. [4], the rate of occurrence of severe psoriasis in children who have facial psoriasis is 4 percent.
We have been following our patient since 2002 and he has not relapsed in this time.
© 2006 Dermatology Online Journal