
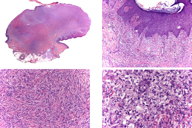
Figure 2. Histological study with a panoramic view and details of fibrohistiocytic cells
A healthy, 34-year-old male presented with a 1-year history of an exophytic lesion on the leg during. On physical examination there was a 2 cm x 3 cm diameter nodule with pinkish, crusted ulceration on its surface; it was attached to skin by a pedicle. It had grown rapidly in the last month. After surgical excision the histological study confirmed the diagnosis of a polypoid dermatofibroma.
A healthy, 34-year-old male presented with a 1-year history of a skin lesion on the right leg that had been undergoing steady growth and causing discomfort. There was no previous history of trauma or injury in the area. On physical examination there was an exophytic tumor of 2 cm x 3 cm in diameter, with erosion and crust (Figure 1). A month later the lesion showed a significant increase in size. Surgical treatment under local anesthesia was performed. Histological sections are shown in Figure 2.
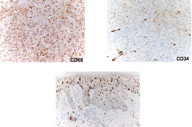 |
| Figure 3 |
|---|
| Figure 3. Immunohistochemical stains showing positivity for CD68, focal positivity for CD34 and CD1A |
Histological examination revealed a well-demarcated and non-encapsulated tumor. The overlying epidermis showed an ulcerated area. In the dermis the lesion was composed of fibrohistiocytic cells interspersed with collagen bundles. Immunohistochemistry (Figure 3) showed focal positivity for CD34 and CD68, but was negative for Melan A and HMB-45. Also there was a high percentage of Langerhans cells in the epidermis (CD1a+). The patient did not suffer any recurrence after 6 months follow up.
Dermatofibroma is a frequent fibrohistiocytic tumor. Clinically its common presentation is a nodule in the dermis located on the lower limbs of a young woman. It usually measures a few millimeters to 2-3 cm in diameter with a slow growing and asymptomatic nature. The color varies from erythematous-brownish to purplish, reddish or yellowish. On palpation it is usually movable at deep levels with a characteristic central depression to lateral pressure (“dimple sign”) [1].
However, there are other forms of presentation. Polypoid dermatofibroma is one of the uncommon clinical forms of dermatofibroma that may be more difficult to diagnose. Polypoid dermatofibroma has an exophytic and pedunculated appearance, a benign biological behavior, and histopathological features similar to conventional dermatofibroma [2]. In our case we noted that focal positivity for CD68, a common fibrohistiocytic antigen, and CD34, an antigen that appears in soft tissue tumors such as dermatofibrosarcoma protuberans [3]. The high positivity for CD1A in the epidermis has not previously been described. The clinical diagnosis of this subtype of dermatofibroma is difficult and the differential diagnosis includes keratoacanthoma, dermatofibrosarcoma protuberans, squamous cell carcinoma, sarcoma, or amelanotic melanoma [4, 5].
There is controversy over the nature of dermatofibroma. Some authors believe that it is a reactive condition of the dermal connective tissue with different stages of evolution and involution. Others assert that it is a benign neoplastic proliferation with a dermal fibrohistiocytic differentiation [1]. According to its evolution and prognosis, the dermatofibroma is a benign growth, although it should be noted that there are some clinical and histological forms with the presence of atypical cells, which may recur and even metastasize [6]. Therefore, the excision should be complete and close monitoring of these patients with these specific subtypes of dermatofibroma should be pursued [7].
© 2010 Dermatology Online Journal