
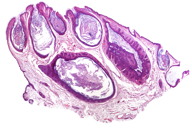
Figure 2. Histopathological exam revealed multiple atrophic cystically dilated hair follicles containing abundant keratinous debris.
A healthy, 5-year-old boy presented with cutaneous lesions on the right buttock, evident at birth. A physical examination revealed plugged pores in a linear distribution with the appearance of comedones and scar areas. Histopathological exam revealed multiple atrophic cystically dilated hair follicles containing abundant keratinous debris and small projections of epithelial cells extending from the wall of the cyst into the surrounding dermis, compatible with nevus comedonicus.
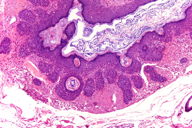 |
| Figure 3 |
|---|
| Figure 3. Small projections of epithelial cells extend from the wall of the cyst into the surrounding dermis. |
A healthy, 5-year-old boy presented with cutaneous lesions on the right buttock, evident at birth. His family history was negative for skin problems. A physical examination revealed plugged follicular plugging in a linear distribution with the appearance of comedones and scar areas (Figure 1). Histologic sections are shown in Figures 2 and 3.
Histopathological exam revealed multiple atrophic cystically dilated hair follicles containing abundant keratinous debris and small projections of epithelial cells extending from the wall of the cyst into the surrounding dermis (Figures 2 and 3). The patient did not exhibit any other associated systemic manifestations. The patient did not require any treatment for aesthetic reasons or complications.
Nevus comedonicus is an uncommon abnormality of pilosebaceous development in which grouped or linear comedonal papules may develop at any time from birth to middle age. It is considered a rare subtype of epidermal nevus. Sometimes inflammation of theses lesions results in severe scarring, fistulae, and sinuses. According to different studies there is an equal sex incidence [1] and no racial predilection. The lesions are typically unilateral, localized, or arranged in zosteriform or linear patterns following Blaschko lines, on the face, trunk, or neck. Scalp, palm, genital area, or wrists are rarely involved. Clinically, nevus comedonicus is of two types. In the first type, comedones are predominantly seen and in the second type, comedones undergo inflammatory changes, with late sequelae such as scars, keloids, fistulae, and formation of follicular cysts [2].
Associated systemic manifestations (comedo nevus syndrome) have been documented. These associations include skeletal (scoliosis, hemivertebrae, spina bifida, polydactyly, et al.), neurological (epilepsy, electroencephalogram abnormalities, transverse myelitis), ocular (cataracts), or cardiac disorders [3]. It can also be associated with other cutaneous disorders such as ichthyosis, trichilemmal cysts, dilated pore of Winer, trichofolliculoma, syringocystoadenoma papilliferum, leukoderma, white hairs, Sturge-Weber syndrome, hemangiomas, and squamous cell carcinoma [4, 5].
The histological features are a large numbers of atrophic cystically dilated hair follicles containing abundant keratinous debris with irregular proliferation into the adjacent dermis. Hyperkeratosis and acanthosis of the epidermis are common findings. The presence of acantholysis and dyskeratosis is regarded as a distinct entity: familial dyskeratotic comedones.
Comedo nevus is a benign lesion and does not need treatment unless the patient requires it for aesthetic reasons or has a complication. Treatment options for nevus comedonicus include antibiotics for inflamed or infected lesions, topical keratolytics, topical retinoic acid (0.025% - 0.1%), 12 percent ammonium lactate lotion, calcipotriene, oral retinoids, dermabrasion, superficial shaving, or surgical excision [1, 6]. Also the use of erbium:YAG and CO2 laser has been reported [7].
© 2010 Dermatology Online Journal