Tumid lupus erythematosus
Published Web Location
https://doi.org/10.5070/D31k03z1tvMain Content
Tumid lupus erythematosus
Macrene Alexiades-Armenakas
Dermatology Online Journal 7(2): 14
New York University Department of DermatologyHistory
This 69-year-old man presented to the Charles C. Harris Skin and Cancer Pavilion with asymptomatic red lesions on his chest of nine years' duration. He did not report pain in his knees and hand joints. He had been treated with hydrocortisone cream in the past with no benefit. He denied fever, chills, weight loss, malaise, fatigue, headache, seizures, oral lesions, hair loss, photosensitivity, or other skin lesions.
Past medical history includes coronary artery disease, atrial fibrillation, hypercholesterolemia, and osteoarthritis. Medications include aspirin, propanolol, digoxin, terazosin, diltiazem, and lovastatin. Family history is negative for skin, rheumatologic, or autoimmune disorders.
Physical Examination
 |  |
| Figure 1 | Figure 2 |
|---|
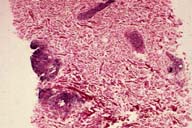
Multiple, smooth, indurated, violaceous plaques and nodules were distributed on the upper chest. The lesions were devoid of surface changes.
Laboratory Data
An anti-nuclear antibody titer was 1:20 with a speckled pattern. Anti-DNA, anti-Sm, anti-RNP, anti-Ro (SSA), anti-LA (SSB), and anti-centromere antibodies were absent. A complete blood count, liver function tests, and urinalysis were normal.
Histopathology
There was a superficial and deep perivascular and peri-adnexal infiltrate of lymphocytes and a few plasma cells. A colloidal iron stain highlighted increased extra-cellular mucin deposits. No epidermal changes were noted. The CD4:CD8 ratio was 3:1.
Comment
Tumid lupus erythematosus is a cutaneous disorder that has been described in the literature mainly as case reports. Until recently, it was often not possible to differentiate tumid lupus erythematosus from other disorders with similar clinically and histopathologic presentations, such as polymorphous light eruption, lymphocytic infiltrate of Jessner and Kanof , pseudolymphoma, and deep gyrate erythema.
A study performed in the Connective-Tissue Section at the Charles C. Harris Skin and Cancer Pavilion using immunohistochemical markers on fresh-frozen skin biopsy specimens now allows us to better distinguish between these disorders. Fifteen patients were prospectively followed over a 14-year period. Smooth, indurated, pink-to-violaceous papules, plaques, or nodules were present on sun-exposed sites for a mean duration of 2.5 years (range two weeks to nine years). The histopathologic changes showed a moderately dense, superficial and deep, perivascular, and occasionally periadnexal infiltrate of lymphocytes. Characteristically, there was an absence of dermoepidermal junctional involvement, although focal changes were observed in a minority of cases. Mucin deposition was demonstrated throughout the papillary and reticular dermis.
Immunohistochemical analysis demonstrated that the infiltrate was comprised predominantly of CD3-positive and CD4-positive lymphocytes whereas a minority were CD8-positive. The ratio of CD4 to CD8 cells was roughly 3:1. In contrast, polymorphous light eruption and lymphocytic infiltrate are characterized by CD8-predominant infiltrates. Thus, in distinguishing between these commonly confused entities, immunohistochemical markers provide important diagnostic information. Based on the results of this study, comprehensive criteria are now available for making the diagnosis of tumid lupus erythematosus. One of the fifteen patients developed systemic lupus erythematosus, which emphasizes the importance of accurate diagnosis, workup and management.
References
Willemze R, et al. Immunohistochemical studies in lymphocytic infiltration of the skin (Jessner) and discoid lupus erythematosus. J Amer Acad Dermatol 11:832, 1984Konttinen, YT, et al. A long-term clinicopathologic survey of patients with Jessner's lymphocytic infiltrate of the skin. J Invest Dermatol 89:205, 1987
Rijlaarsdam JU, et al. Characterization of the dermal infiltrates in Jessner's lymphocytic infiltrate of the skin, polymorphous light eruption and cutaneous lupus erythematosus: differential diagnostic and pathogenic aspects. J Cutan Pathol 17:2, 1990
Akasu R, et al. Lymphocyte markers on formalin-fixed tissue in Jessner's lymphocytic infiltrate and lupus erythematosus. J Cutan Pathol 19:59, 1992
Dekle CI, et al. Lupus tumidus. J Am Acad Dermatol 41:250, 1999
Kuhn A, et al. Lupus erythematosus tumidus: a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol 136:1033, 2000
© 2001 Dermatology Online Journal

