Skip to main content
Dermatopathology Unknown:

References
Dermatopathology Case: Perianal lesion of three weeks duration.
Published Web Location
https://doi.org/10.5070/D365z230tzMain Content
Dermatopathology Unknown:
A 58 year old woman with a perianal lesion
Ronald J. Barr, M.D.
Dermatology Online JournalVolume 2, Number 1: 7

Clinical History:
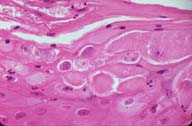
A 58 year old Mexican woman presented with a three week history of a perianal lesion.Important Microscopic Features:
- Irregular and veruccous acanthosis
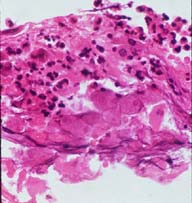
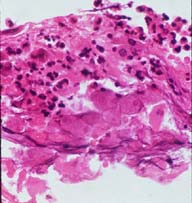
- Superficial crusting with superficial necrosis
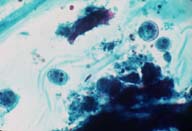
- Characteristic trophozoites of Entamoebea histolytica: These appear as round, mononuclear cells with granular, grey-blue cytoplasm. The nucleus has a centrally located karyosome. Most are loculated within areas of superficial crusting and a few contain red blood cells.
Differential Diagnosis
- Condyloma acuminatum
- Condyloma latum
- Verrucous carcinoma (The identification of the characteristic trophozoites is pathognomonic for amebiasis cutis).
Diagnosis: Amebiasis cutis
Comments(1)
Cutaneous amebiasis, unlike gastrointestinal (GI) tract amebiasis, is a rare condition and occurs chiefly in the tropics.(2) Cutaneous lesions arise from the direct extension of GI tract amebiasis, from surgical intervention (producing lesions at the incision site), from primary infection of the skin, from venereal transmission, or from metastasis after parasitemia.(3) Cutaneous lesions have been reported to occur on the trunk, buttocks, perineum, genitalia, and legs. Amebic ulcers are oval with irregular, necrotic, ragged, or verrucous borders that extend peripherally and rapidly with increasing toxemia. Subcutaneous swellings called "amebomas" may also occur. Skin lesions develop most often in patients in poor general health as a consequence of fistulous extension from a GI tract or hepatic abscess. The cutaneous amebiasis that developed in our patient, who was otherwise in good health, probably was a result of direct extension from asymptomatic intestinal amebiasis.Cutaneous amebiasis may be preceded by diarrhea, dysentery, or the passing of mucus. Saline mounts of skin scrapings of the lesion or a biopsy specimen from the ulcer edge will demonstrate trophozoites and confirm the diagnosis.
References
- Fujita WH, Barr RJ, Gottschalk HR: Cutaneous Amebiasis. Arch Dermatol 117:309, 1981.
- el-Zawahry M, el-Komy M: Amoebiasis cutis. Int. J. Dermatol. 12:305, 1973.
- Majmudar B, et al: Amebiasis of clitoris mimicking carcinoma. JAMA, 236: 1145, 1976.
All contents copyright © 1996. Dermatology Online Journal University of California Davis