Pyogenic granuloma arising in port-wine stain after cryotherapy
Published Web Location
https://doi.org/10.5070/D35wj259vvMain Content
Pyogenic granuloma arising in port-wine stain after cryotherapy
Shahin Aghaei MD
Dermatology Online Journal 9 (5): 16
Department of Dermatology, Shiraz University of Medical Sciences.shahinaghaei@yahoo.com
Abstract
Pyogenic granuloma is a reactive vascular tumor that rarely arises in association with port-wine stain, either spontaneously or after trauma. A 21-year-old woman, presented here, developed a pyogenic granuloma within a facial port-wine stain after treatment with cryotherapy.

|

|
| Figure 1 | Figure 2 |
|---|---|
| Red patch on the right side of the face, a port-wine stain (Fig. 1). Erythematous papule that developed within the port-wine stain following cryotherapy (Fig. 2). | |
A 21-year-old female presented with a 0.5 cm erythematous papule on the face (Figs. 1 and 2). The papule was located within a well-demarcated red patch, a port-wine stain (PWS) that had been present since birth on the right side of the face. The PWS had undergone several CO² laser treatments without improvement. Some 12 months after completion of laser therapy, cryotherapy with a cotton-tipped applicator was begun to selected sites. She had significant improvement after 24 weeks of cryotherapy administered once per week. After 25 weeks of cryotherapy an enlarging papule was noticed in the PWS. The papule was nonpruritic but bled spontaneously and with mild trauma. Shave excision of the papule was followed by electrodesiccation.
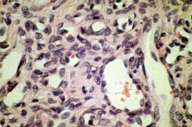
The histopathology of the lesion showed a polypoid papule composed of numerous dilated capillaries in a lobular pattern. The stroma showed an increase in pericytes and an acute and chronic inflammatory infiltrate. These findings were consistent with the diagnosis of pyogenic granuloma (PG). She had not developed PG with CO² laser therapy.
|
|
| Figure 3 | Figure 4 |
|---|---|
| Histopathology of the lesion. Original magnifications 40× (Fig. 3) and 300× (Fig. 4). | |
Discussion
PG rarely occurs in association with PWS, either de novo or following trauma such as laser therapy. One explanation attributes its development to microscopic arteriovenous anastomoses. This explanation is supported by the predilection of PG for acral sites after trauma, and by the association of PG with arteriovenous hemangiomas [1]. PGs and PWSs are vascular lesions that rarely occur together despite their distinct clinical, histological, and biological differences [2]. In previously reported cases of PGs arising on PWSs, the patients had undergone several laser treatments, known to be predisposing factors [1, 3]. Other predisposing factors are pregnancy [3, 4], oral contraceptive pills [5], minor trauma [1, 6, 7], smallpox vaccination [8], and hair transplantation [9]. The majority of PGs, however, arise spontaneously [2], even though PG is regarded as a reactive tumor rather than a neoplasm [10].
The development of PG in this patient probably resulted from the presence of an underlying arteriovenous anastamosis associated with the PWS, combined with external trauma in the form of cryotherapy.
PWS, which is a vascular malformation, and PG, which is a vascular tumor, arise via different processes; their regulatory mechanisms are complex and under study [2]. A literature review revealed only three other reports describing an association between cryotherapy and PG. Unlike this case in which the PG appeared within a PWS, the primary lesions in the previously reported cases were verruca vulgaris [11] and venous lake [12].
It is also interesting that this patient's PWS responded favorably to gentle and repetitive cryotherapy, although the current treatment of choice is considered to be pulsed-dye laser [13].
Acknowledgment: I thank Dr. Farhad Hanjani for his assistance. I acknowledge Dr. Ahmad Monabbaty from Department of Pathology, Shiraz University of Medical Sciences.
References
1. Lee JB, Kim M, Lee SC, Won YH . Granuloma pyogenicum arising in an arteriovenous haemangioma associated with a port- wine stain. Br J Dermatol 2000; 143: 669-70.2. Garzon MC, Enjolras O, Frieden IJ . Vascular tumors and vascular malformations: evidence for an association. J Am Acad Dermatol 2000 Feb;42(2 Pt 1):275-9. PubMed
3. Lanigan SW, Cotterill JA . Pyogenic granuloma , port- wine stains and laser therapy. Lasers Med Sci 1988; 3:7-11.
4. Katta R, Bickle K, Hwang L. Pyogenic granuloma arising in port-wine stain during pregnancy. Br J Dermatol 2001; 144:644-45.
5. Mussalli NG, Hopps RM, Johnson NM . Oral pyogenic granuloma as a complication of pregnancy and the use of hormonal contraceptives . Int J Gynecol Obstet 1976; 14: 187-91.
6. Suzanne VG , John BM . Vascular anomalies. In : Dermatology in General Medicine (Fitzpatrick TB, Irwin MF , Arthur ZE et al. ,editors), 5th ed. , Vol 1. New York : McGraw -Hill Inc., 1999:1183-4.
7. Michaelson HE. Granuloma pygenicum . A clinical and histological review of 29 cases. Arch Dermatol 1925; 12:119-28.
8. Zayid I, Farraj S. Granuloma pyogenicum- a hitherto unrecognized complication of smallpox vaccination . Br J Dermatol 1974; 90:293-9.
9. Sarnoff DS, Goldberg DJ , Greenspan AH et al . Multiple pyogenic granuloma-like lesions following hair transplantation . J Dermatol Surg Oncol 1985; 11:32-4.
10. Eduardo C, Edward WJ . Vascular tumors. In : Histopathology of the skin (Lever WF, Elder D, Elenitsas R et al. , editors), 8th ed. Philadelphia : Lippincott- Raven Co.,1997; 895-7.
11. Kolbusz RV, O'Donoghue MN. Pyogenic granuloma following treatment of verruca vulgaris with cryotherapy and Duoplant. Cutis. 1991; 47(3):204. PubMed
12. Cecchi R, Giomi A. Pyogenic granuloma as a complication of cryosurgery for venous lake. Br J Dermatol 1999; 140(2):373-4.
13. Hansen K, Kreiter CD, Rosenbaumm, Whitaker DC. Long-term psychological impact and perceived efficacy of pulsed-dye laser therapy for patients with port-wine stains. Dermatol Surg 2003; 29(1):49-55.
© 2003 Dermatology Online Journal

